Questionnaire
The CallingCOVID.com Questionnaire - Introduction
Thanks for visiting! To translate this page, select your language from the dropdown menu below:CallingCOVID.com
Assessing the impact of long term COVID-19
- "Sharing" first and most importantly with the patients themselves.
- Responses provided are anonymous so that "sharing" may also include any and all who have the intention of contributing to healing those with this illness.
- More is known at present than months ago. It is less "novel" but much about this illness is different and much remains unknown or unexplained.
- Hopefully, responses here will help to usefully fill the void that remains while encouraging compassionate care.
- Who is doing this?
Your answers will serve :
- to allow comparisons with others who have this illness
- to provide insights for those who are faced with the task of curing this illness
- to gather together in one place, through your responses, a piece of what is known
- to give those affected with this illness a timeline for recovery
- to suggest what is still unknown, and serve as an incentive to further learning
- to provide clues as to what works, to move all who are ill towards recovery.
Who gets the responses ?
- First and foremost, those who gave the answers ! After completing the Questionnaire, you get to see how others answered up to that time and date.
- Anyone who has this illness and wants to know more. Answers will be presented here on this site in an easy to understand format. If you are going to respond to our questionnaire, it makes sense to only review how others answered after ! It's not a test. There are no right answers.
- Anyone who can communicate a project or protocol they are working on, and which would benefit those still suffering with COVID-19, could get the results. Results would not include any identifying information from respondents. When feeling poorly, no one needs a call or emails from a drug salesperson.
About the Questionnaire
- It attempts to be thorough, inclusive and thereby provide good and adequate information.
- So it's not 3 questions. Including our final Thank You!, it's 59 questions.
- Those where the questionnaire is managed (SurveyMonkey), suggests it takes 27 minutes. That will seem long to some. To others reasonable, given the large amount of information obtained. What else can we say?
- Well, we can say: "Have a look!" And soon, it will be translated into other languages.
- Don't expect to find hundreds of responses presented here today or tomorrow. It's formulation was in early September, put into use 12 Sept., and as of 19 October, 113 individuals with presumed "Long-term" COVID-19 had responded. (Thanks again to these for their participation!)
- Answers to the Questionnaire will be posted on this page. <<<<<<<<
- As of October 19, 10 preliminary reports have been provided about results of testing, changes in weight, sources of emotional support, resilience, quality of life perceptions, the balance of physical and emotional symptoms, levels of limitation of physical activity, and other analyses of answers provided. Through these, a better understanding of how "long-term" COVID-19 actually presents, begins to come into focus. These are the patients telling their story. Thanks again!
Why is it on this site ?
- Because CallingCOVID.com intends to do just that. To call out to those still with active disease, but also to those who are (thankfully) better, even if it took a while. They are now experts, and their advice and experience are needed to move others towards healing.
- Those with Long-term COVID-19 or "long-haulers" will soon be a Target for the Challenge, which you can read about in many places on this site. Perhaps best starting here.
Lesson 8: How much does "Long-term" COVID-19 impact one's usual activity level?
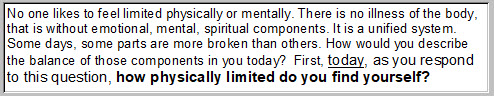
Question 42 of our questionnaire addresses that. Here's how the question was phrased:
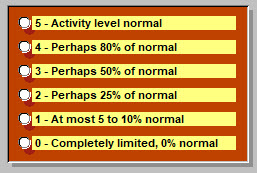
And the point of reference was at the time of taking the questionnaire. At that point, most respondents had been ill about 6.5 months. Possible answers were:
Level of activity of course depends on how sick one is. One can readily imagine a person with a cold, moving through his day, blowing his nose and complaining about how he feels. (While spreading around his cold). But with an activity level perhaps not too abnormal. That's just an example.
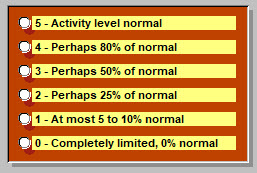
Already presented elsewhere, here is a reminder about illness severity, the responses to Question 28:
A bit hard to read, but 79% (of 100 respondents as of 7 October) placed this as a moderate illness, "very sick, many symptoms, lasted longer than anticipated." So no, not a cold.
But how much did this physically limit those affected?
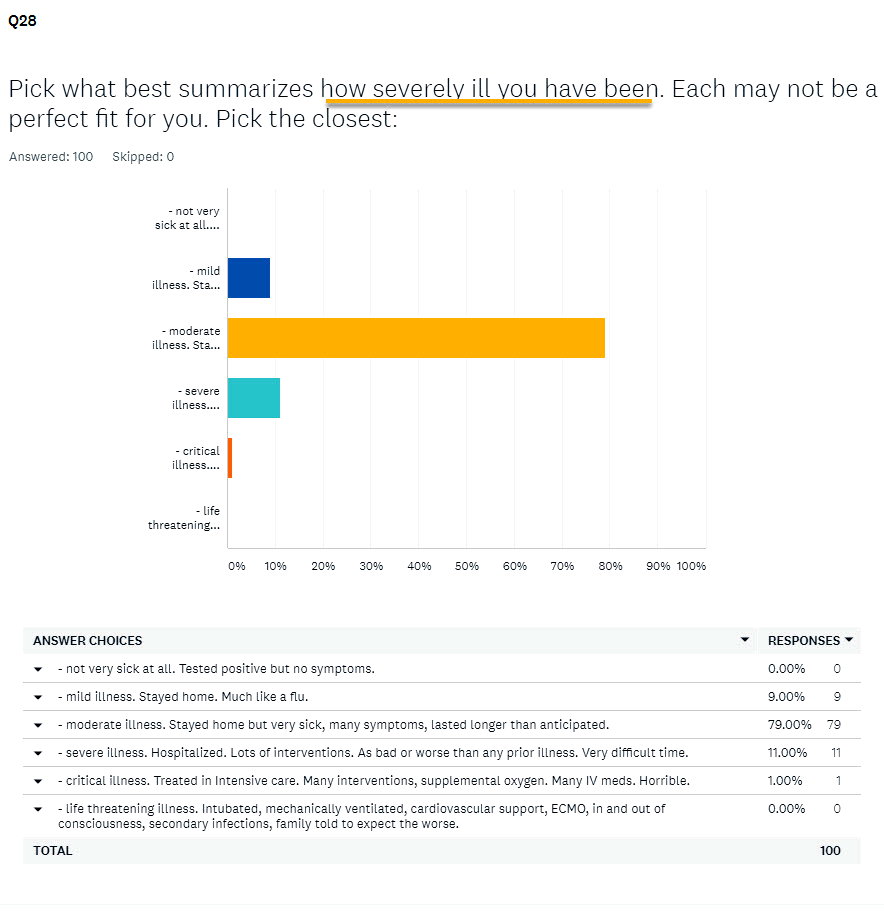
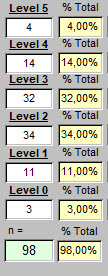
Here, in the column at right, are the answers obtained:
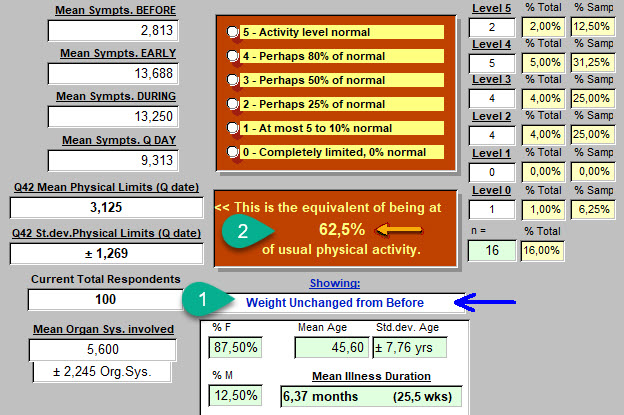
As frequently happens, some questionnaires (2 in this case) were omitted because of too many inconsistencies in dates or ommissions of information (like gender, DOB, etc). So 100 responses became, n = 98. The column with percentages at right is based on the total of 100 nevertheless. The distribution of responses from highest to lowest seems pretty "normal" which has a specific meaning for subsequent statistical analysis.
These results permit calculation of a mean or average value, which looked like this on this date.
On the left below, the mean and standard deviation (amount of variability around that mean value).
As one can see, by translating that into a percentage of the highest score possible (5) we learn that this illness in its "long-term" variant, cuts usual physical activity essentially in half.
"... how physically limited do you find yourself?" was being asked: and the answer is clear.
Some people are usually more physically active than others of course. And does this illness affect differently what we can identify as subgroups of this larger group of 98 on this day?
What about effects of age? What about gender differences? How about habits one had before becoming ill, such as smoking or taking nutritional supplements? What about one's size: Underweight? Overweight? Obese? We'll look at some of these next.
But first a caveat. To find very subtle differences between two such subgroups, say women and men, and effects of this illness on activity levels, a more robust number of respondents than n=98 may be necessary. That's a plug for getting the questionnaire into more hands of those with this illness. And the word of caution serves to remind that subtle differences may get exactly reversed when "n" has increased substantially.
That said, statistical control of these results is possible already, and where clear differences are already discovered to be significant, those may persist with larger numbers as well. And the results already suggest some quite interesting possibilities, as seen further below.
First, some less proounced differences.
What about gender?
90.82% of respondents are female, so 9.18% male. What levels of activity compared with "usual"?
Female: 52.1% Male: 51.1% One guesses at "no difference." Once can compare means ...
Female: 2.604±1.138, n = 91 with Male: 2.556±0.831, n = 9. The answer takes the form of a probability that this slight increase in activity level among women, is different than that for the 9 men respondents. p=0.9023, and that means that 90 times out of 100, that 1% apparent difference just isn't real.
Conclusion: men and women are equally impacted in activity levels by this illness.
What about age?
Those respondents <= to age 49 years, (n=47) have an activity level result of 51.1%
Thos older than 49 years (n=53) "score" 52.8% of usual activity level. Answer? Nope. A value of p=0.6906 informs that this slight difference is probably imaginary 69 times out of 100 times that you would gather the data.
Yes, one finds subgroups of age that seem more or less affected. The differences are too small to be important on this date. But with another 5000 respondents, who knows?
Conclusion: those of all ages are equally impacted in activity levels by this illness. Of course, as presented above, this is a moderate illness for most. If only those critically ill had answered, age might become a quite important determinant of activity level. Here, those data are absent.
What about weight? Does a person's size, reflected in the Body Mass Index, make a difference in activity levels when compared with usual activity?
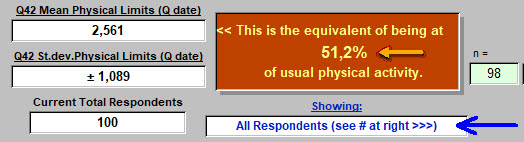
92 of the 98 with useful answers provided Height, Weight Before, and Weight on the day they responded. Once different units had been converted to metric, that looked like this:
Weight changes and perhaps related to a direct effect of the virus on adipocytes (fat cells) have been covered before in another article. In fact two articles. We see here that 45.7% of those who responded, gained weight. But what about a possible effect of body size and changes in size, on activity levels?
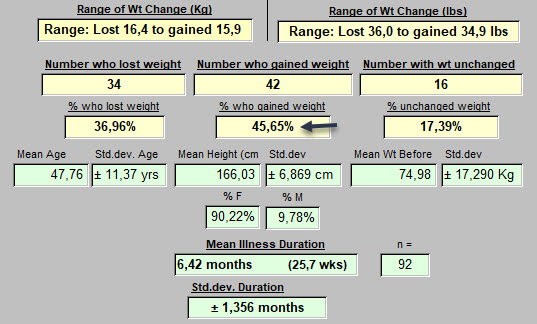
Here are those who serve in some sense as controls: no change in weight while sick.
Lots of other numbers on this image, but concentrate on point 1 below: "Weight unchanged from before." and point 2: 62.5% of normal activity level. So that's better (a bit closer to normal) than the average we saw at the top of this page (51.2%).
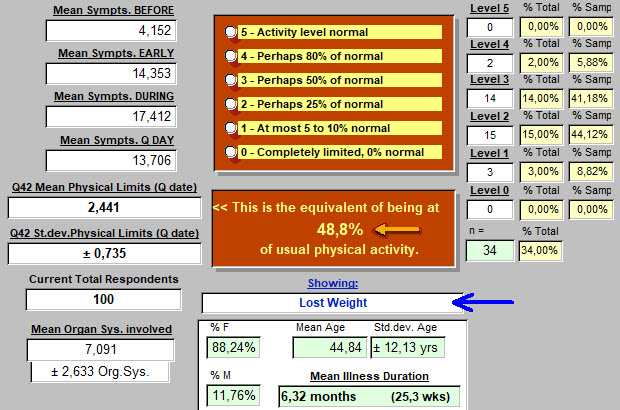
Those who lost weight while ill: 48.8% of usual activity level.
Is this a different result than for those who's weight did not change?
The null hypothesis is that there is no difference in these activity levels.
Answer is: p = 0.0197, so this hypothesis of "no difference" is not sustained. About 2 chances in 100 tries that we'd come up with a different conclusion.
Conclusion: Weight loss during this illness is accompanied by a significant reduction in activity level, when compared with those who's weight remained unchanged during the illness.
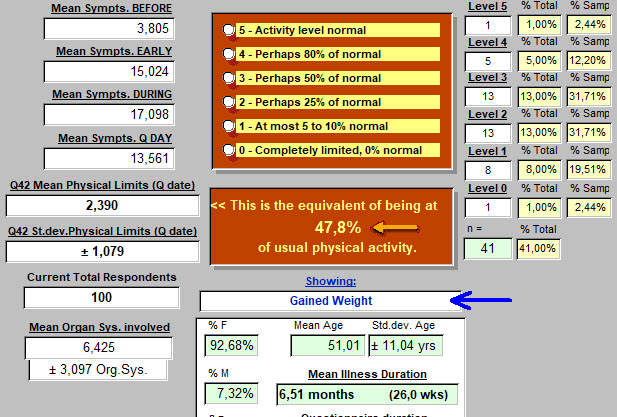
Those who gained weight while ill: 47.8% of usual activity level.
Is this a different result than for those who's weight did not change?
The null hypothesis is that there is no difference in these activity levels.
Answer is: p = 0.0321, so this hypothesis of "no difference" is not sustained. About 3 chances in 100 tries that we'd come up with a different conclusion.
Conclusion: Weight gain during this illness is accompanied by a significant reduction in activity level, when compared with those who's weight remained unchanged during the illness.
Let's quickly pass over other possibilities related to weight or more accurately, Body Mass, and possible effects on level of activity when compared with usual levels before illness.
Again, where the differences are subtle, as more respondents add to replies, the conclusion may in fact become reversed, even if usually more certain. Preliminary results are presented here at a point in time. Many will be close to the mean value for limitation of physical activity by this illness. Others, may be a bit more remarkable.
| Before vs on Questnr. date | Percent of Usual Physical Activity | Number of respondents (n) |
| Those Underweight and still are | 46.7% | 3 |
| Obese before | 47.2% | 25 |
| Class 3 Obese before & still | 30.0% | 4 |
| Obese before but no longer | 40% | 6 |
| Not obese before, became so | 40% | 3 |
| Not Overweight, became so | 60% | 7 |
What about other components of health status, that might have some link to how well physical activity levels are maintained?
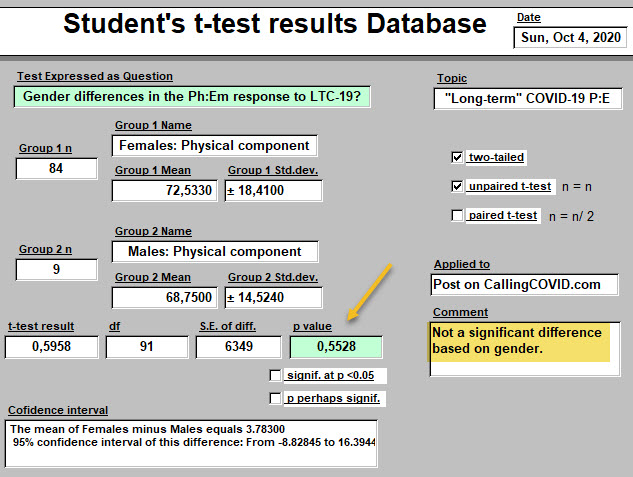
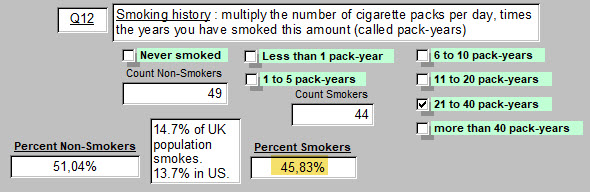
What about smoking?
In the UK, 14.7% of the population smokes. That figure in the United Sates is 13.7% (2019 figures).
In our sample of 100 respondents on October 7, 46 have a smoking history. That is of course 46%.
So what might one think about the potential effect of a history of smoking on physical activity levels when one is now ill with "long-term" COVID-19? Is there any effect at all?
Here are the results from this sample. On this day, with 100 respondents each number, 'n' , is also the percentage:
| Smoking History | Percent of Usual Physical Activity | Number of respondents (n) |
| Never smoked | 47.8% | 54 |
| Those who smoked | 57.0% | 46 |
|
Moderate smokers |
58.3% | 24 |
| Heavy smokers | 54.3% | 21 |
| Women, never smoked | 47.5% | 48 |
| Women, smokers | 55.6% | 41 |
| Men, never smoked | 44.0% | 5 |
| Men, smokers | 60.0% | 4 |
It looks like, if one is a non-smoker, one should quickly take up the habit in support of improved physical activity levels !
Let's put some to the test. Using their means and standard deviations:
Non-smokers: 2.389±1.145, n=54
All Smokers : 2.848±1.021, n=46
The test is Student's t-test, unpaired, two-tailed.
The null hypothesis is that their is no difference in physical activity levels of these subgroups of "long-term" COVID-19 patients.
Result: t = 2.0991 df = 98 standard error of difference = 0.219 p = 0.0384
Conclusion: the null hypothesis of no difference is rejected. Smokers with this illness maintain a level of physical activity that is closer to their baseline, and superior to non-smokers.
For Moderate Smokers, also essentially true. 2.917±1.077, n=24, p=0.0595
For Heavy Smokers, less true, 2.714±0.933, n=21, p=0.2505, so not a significant difference.
Women, Never Smoked: 2.375±1.148, n=48
Women, +ve Smoking Hx: 2.780±1.024, n=41
Null hypothesis: no difference in mean level of limitation of physical activity, based on smoking or not in these female respondents presenting with "long-term" COVID-19.
Result: t = 1.7428 df = 87 standard error of difference = 0.232 p = 0.0849 (close but no cigar).
9 chances in 100 tries that there is no difference. Some would still bet on their being a difference.
As more respond, the conclusion may change.
Men, Never Smoked: 2.200±0.980, n=5
Men, Men, Smokers: 3.000±0.001, n=4
Results for these very small subgroups, p=0.1515
Positive Health Habits
In presenting observed effects of body size and smoking on physical activity levels of respondents, one introduces a related topic: doing what one can to maintain one's health. Maintaining a normal weight. Not smoking, or quitting.
What else might one choose to do in support of one's health?
And do such choices specifically impact how well physical activity is preserved when, unfortunately, one is ill with "long-term" COVID-19?
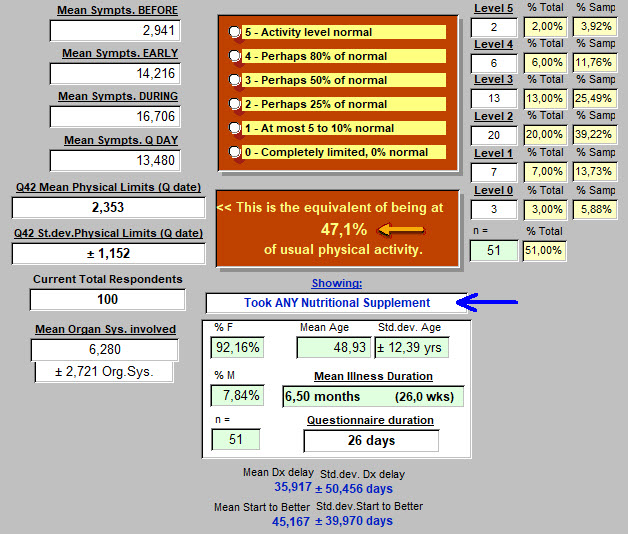
We'll look first at respondents who took any form of Nutritional Supplement.
And subsequently: Vitamin-D is again "in the News." This time for protecting against and perhaps for treating respiratory problems of COVID-19. How were respondent Serum Vit-D levels before becoming sick? How much Vitamin-D were they taking before? We'll look at that as well. All of this couched in terms of effects on effectiveness of reducing physical limitations during this illness.
Of course, results of pursuing such information might be expected to be quite different in a population of respondents who are competitive athletes, and a group presenting chronic health problems.
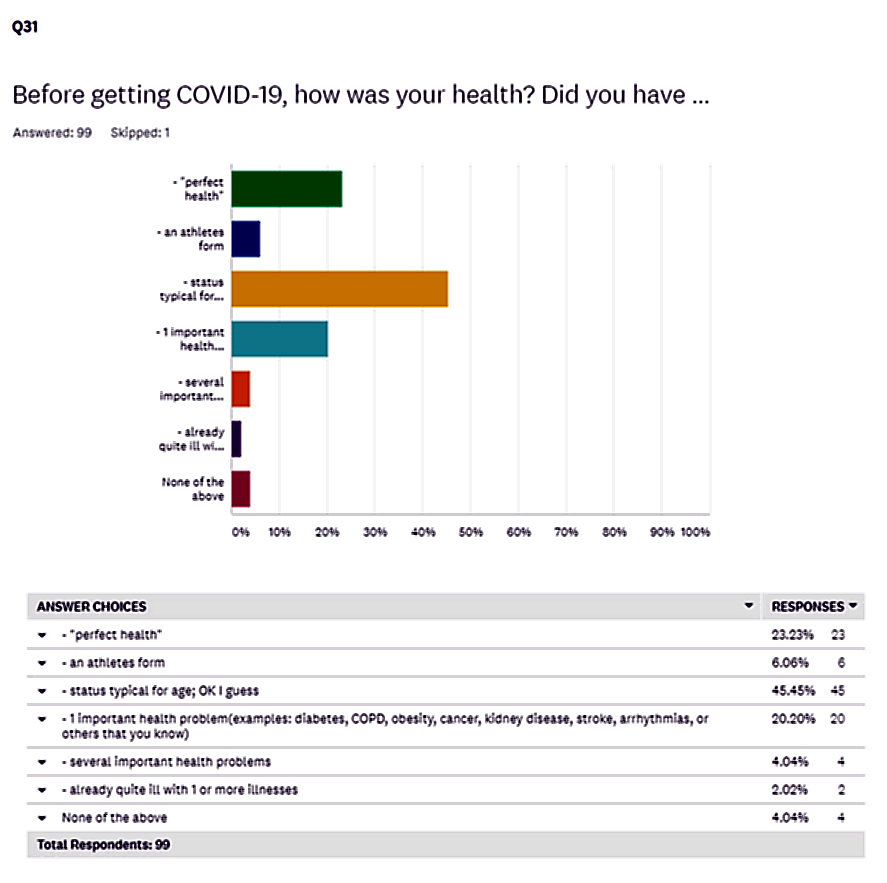
So how "healthy" was our group of 100 respondents before they became ill?
Question 31 of the questionnaire provides that answer:
So the majority (46%) presented through their choice, a status typical for age. Athletes, only 6%. Twenty-three percent selected "perfect health," and 20% with 1 important health problem before catching COVID-19.
Nutritional Supplements
Did respondents take these, and what was the impact on Physical Activity Limitations on the day they responded to the questionnaire?
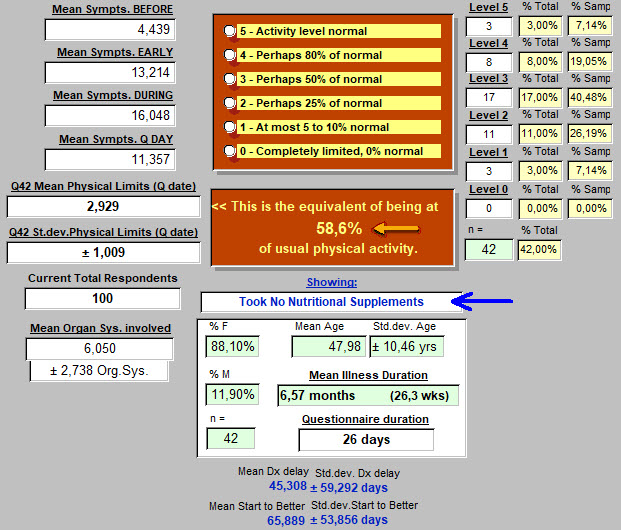
Here below, lots of numbers. So stay focused on those two in the middle with the arrows ...
Those who took No Nutritional Supplements, 42 respondents, had an average physical activity level at 58.6% of their usual level on the day they took the questionnaire.
How about those who responded that they took some form of nutritional supplement? That might be one multivitamin each day, or some added protein, or some Vitamin-D of varying doses, or several vitamins and supplements each day. For this response, all are equated with taking a nutritional supplement.
Again, for the question at hand, focus on the arrows in the middle.
Those who took ANY Nutritional Supplements, 51 respondents, had an average physical activity level at 47.1% of their usual level on the day they took the questionnaire.
"Oh No! More people take nutritional supplements than don't, and they did worse!"
If that is the hypothesis, is it true?
Or is it actually that no difference exists in mean physical activity limitation level of these two groups?
Answer is: The two-tailed P value equals 0.0129 The idea of no difference is rejected.
Conclusion: Those (42) presenting with "long-term" COVID-19 who reported taking No Nutritional Supplements at all, maintained a higher level of their usual physical activity, than those (51) who took Any Supplement. Possibility that this conclusion is wrong? 13 chances in 1000 trials.
Vitamin - D Supplements
Since we are still hearing that Vitamin-D may play a protective role against respiratory complications of COVID-19, might taking that supplement routinely before getting sick, also impact on Physical Activity Levels?
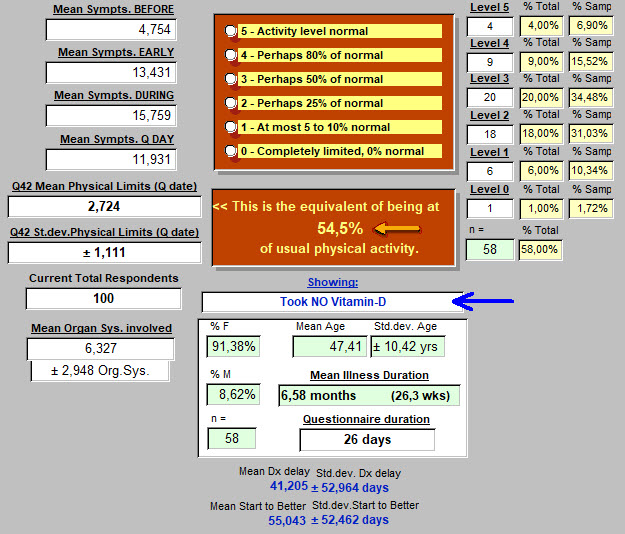
Here below, no one took supplemental Vitamin-D.
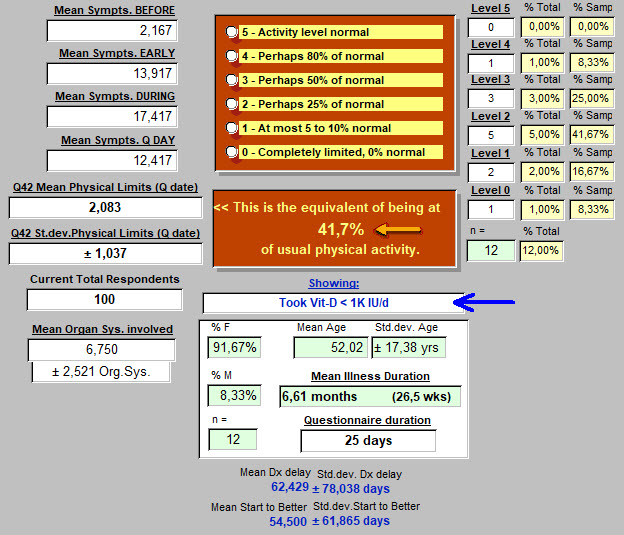
And here below, respondents took Vit-D, but less than 1000 IU per day:
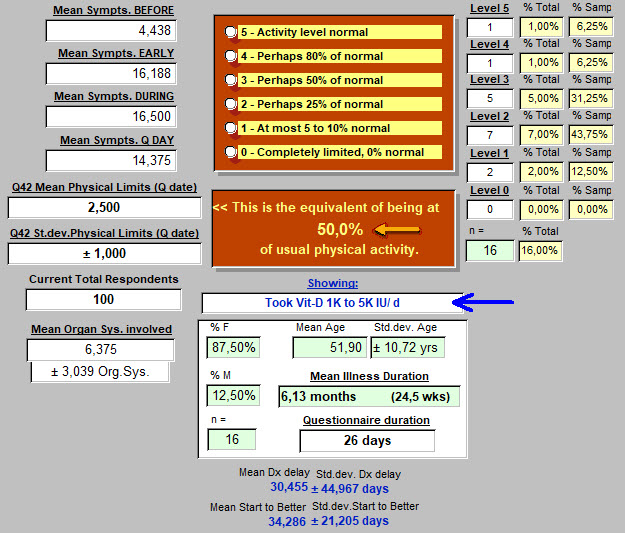
And finally, respondents taking between 1000 and 5000 IU Vitamin-D each day:
Results:
- Those (58) taking no Vitamin-D seemed to better maintain physical activity than those (12) taking low doses of less than 1000 IU per day. The two-tailed P value equals 0.0704. Almost a significant difference at the usual p<0.05 level. So probably already suggesting something that will become more apparent with more respondents who take small doses of the vitamin.
- For those taking larger (1000 to 5000 or more IU of Vit-D per day), compared with those taking none, the two-tailed P value equals 0.4686. This means that no difference was found in the physical activity levels of these two groups, no Vit-D vs. higher dose Vit-D.
- Comparing level of limitation of physical activity of the low dose (12) vs. higher dose Vit-D (16): The two-tailed P value equals 0.2923. So 29 chances out of 100 that any apparent difference arose by chance.
This is not saying that taking supplemental Vitamin-D serves no purpose. But as related to level of physical activity limitation due to "long-term" COVID-19, no beneficial effect was discovered so far in these preliminary results.
How about measured blood levels of Vit-D? They may be a better gauge of how much Vitamin-D is getting into the body. Of those responding, how many had serum Vitamin-D levels that were below normal, and how many at or above normal? And to keep focus for this article, were there significant differences in levels of limitation of physical activity associated with these blood levels of this specific supplement?
Results:
- Serum Vit-D reported as below normal (n=10), and at or above normal (n=5). Those below normal maintained an average of 56% of activity while those at normal and above averaged 40%. The two-tailed P value equals 0.0966. By conventional criteria, this difference is considered to be not quite statistically significant. But with these small group sizes no conclusion should be drawn at this point. Why would a higher Vitamin-D blood level be detrimental to physical activity?! Doesn't fit with what is already well established in the medical literature about this substance.
----------
A final comparison may reveal some intriguing aspects of this illness that emerge from these preliminary results of our questionnaire.
Some respondents provided no date when they were diagnosed with COVID-19.
Some respondents have had no positive tests confirming COVID-19.
Other respondents provided a date when told that they "had COVID-19" and at least one positive test. Many had several positive tests.
So how do these groups compare in level of limitation in Physical Activity?
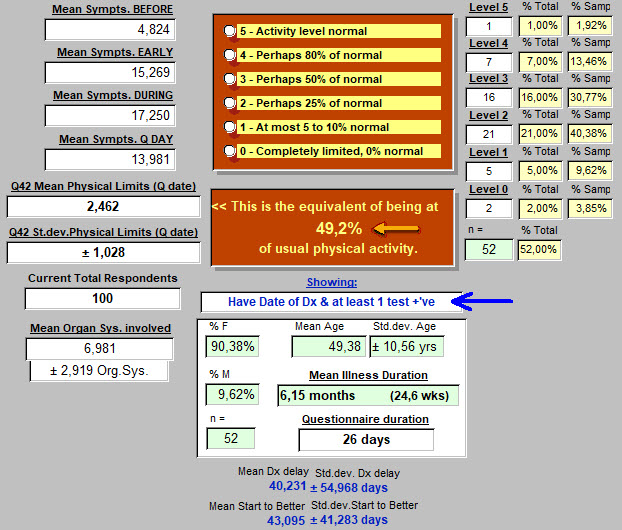
First, those with a date of diagnosis (Dx) and at least 1 positive test for COVID-19.
They are at an average of 49.2% of usual physical activity.
Again, on the image below, we are focusing on the two central points with arrows:
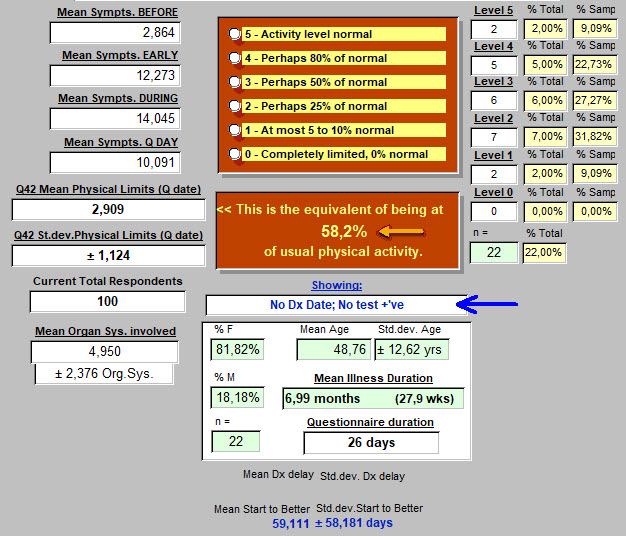
And below, those who provided no Date of Diagnosis and not a single positive test (including physical exam alone) : average Physical Actvity level - 58.2% of normal.
Staying focused on Physical Activity Level, the null hypothesis says that there is no difference in this level for these two subgroups of our 100 respondents.
Dx date & +'ve test: 2.462±1.028, n = 52.
No Dx date or +'ve test: 2.909±1.124, n = 22.
t = 1.6629 df = 72 The two-tailed P value equals 0.1007. Or, 10 chances out of 100 that there is no difference. Probably on to something. Are those with No Date of Diagnosis, and No Positive Test, and who seem to be doing better physically after the same duration of illness, ... just making it all up? Probably not. But this may be defining a subgroup or variant of the COVID-19 illness. Or perhaps, they have a completely different illness? Fungal disease, such as Aspergillosis comes to mind.
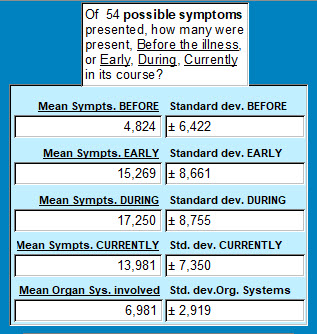
If one compares average number of symptoms reported Before, Early in illness, During the illness and on the day of the Questionnaire, here are the values for those WITH a Date of Diagnosis and Test Pos. :
90.38% female, 9.62% male, age 49.38±10.56 years, ill 24.6 weeks.
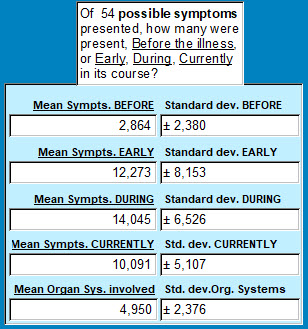
And for those WITHOUT a Dx Date and no positive test :
81.82% female, 18.18% male, age 48.76±12.62 years, ill on average, 27.9 weeks.
Simply put, those with no Dx Date nor a Pos. Test report fewer symptoms throughout the course of this illness, and even Before the illness began.
BEFORE: The two-tailed P value equals 0.1697
EARLY: The two-tailed P value equals 0.1709
DURING: The two-tailed P value equals 0.1273
CURRENTLY: The two-tailed P value equals 0.0270**
Organ Systems Involved : The two-tailed P value equals 0.0052***
Results: reported symptom count before, early in the illness, and throughout the illness, though seemingly higher in the group with Dx Date and Pos. Test(s) were not statistically different from the other group who provided no Date of Dx nor any positive test results.
But at the time the questionnaire was completed, the number of symptoms was now different and higher in the group with Dx Date and Pos. Test(s). Only 3 chances in 100 that this apparent difference was not real.
The apparent difference in the reported count for Organ Systems involved (on average, 6.98 vs 4.95) is even more significant. Five chances in 1000 that this apparent difference arose by chance or error.
----------
CONCLUSIONS :
-
- "Long-term" COVID-19 patients have a significantly limited level of physical activity when compared with pre-illness levels. Essentially, cut in half.
- To obtain these results, nothing was objectively measured here, other than the respondent's subjective opinion. Of course, if someone reported taking a dose of 5000 IU of Vitamin D, it was accepted as an objectively true and accurate response. Being objective and accurate about one's activity level may be a bit more difficult. We did not measure hand grip strength or number of pushups at 4 different times.
- This level is at approximately 50% of where they were before becoming ill. That requires time and resilience to adapt to. On a scale of 0 to 5 for resilience, these 100 respondents averaged 3.521±1.216. This was between the two responses of: "Don't know yet. Scared and stuck on many days. Always hopeful. Not resilient yet." (value 2) and "I usually bounce back, but this was a blow. I do feel I'm slowly recovering some resilience." (value 3). Resilience was explored in Question 56, and has been addressed in a separate article.
- Certain factors in place before developing the "long-term" COVID-19 illness are also determinant of this limitation of activity level.
- those who were underweight, and
- those who were Class III obese have more problems with physical activity limitations
- smokers may have less physical activity limitations than non-smokers. Not intuitive, but probably true. Prompts a search for explanation(s).
- Taking supplements (before becoming ill with COVID-19), either in a general form like "multi-vitamins" or specifically, Vitamine-D, did not contribute to maintaining a higher level of Physical Activity while still ill with "long-term" COVID-19, when compared with normal Physical Activity levels for each respondent before becoming ill.
- The subset of respondents (22, or 22% at this time) who provided no Date of Diagnosis of COVID-19, and no positive tests to support this diagnosis is interesting. They have fewer symptoms than the paired group with positive diagnostic results. This is only supported statistically at the time when they responded to the questionnaire. Yet, they have many symptoms as well. At the time of taking the questionnaire, they clearly have fewer symptoms. And the number of organ systems involved is certainly less. As demonstrated, the limitation of Physical Activity is less in this group lacking the usual diagnostic information. Explanation? None that is clear. Are they less ill than the group supplying diagnostic information? Probably. A higher percentage of males, though still mostly female as in the other group. They are also further along in the duration of the illness when they responded. Are they just closer to "being better"? Does this explain fewer symptoms? Not for those times identified as Before, Early, and During. Are they a variant of this "long-term" COVID-19? Possibly.
Closing thoughts:
Frequently, the respiratory and less commonly the cardiovascular systems are involved with COVID-19.
A pulse oximeter on a finger is a commonly presented image.
Smokers are inflicting upon themselves, a chronic level of hypoxemia, and from that, tissue hypoxia.
Their tissues become more adept at extracting oxygen from hemoglobin, and living in a somewhat desaturated condition.
In those with pre-existing obesity, meeting tissue oxygen demands is also a chronic problem. It is challenged by routine physical activity each day when climbing stairs for example.
So in fact, these two subgroups presented here represent a state of chronic relative tissue hypoxia.
It is somewhat akin to living at higher altitudes. Initially challenging but eventually leading to physiologic changes to avoid having hypoxemia (reduced O2 levels in the blood) become tissue hypoxia (reduced levels of O2 at a cellular level).
One might consider these both as a form of training for the oxygen-related deficits seen in COVID-19.
As odd as that sounds, those who never smoked are not chronically on the borderline of tissue hypoxia. Those who were not carrying around excess weight, had no reason to make physiologic adjustments to assure adequate oxygen delivery. Then the oxygen delivery problems associated with this viral illness came into play. And without "prior training." More effects that lean towards limitation of physical activity.
Those at the extreme ends of underweight or overweight, have a marked limitation of physical activity imposed by this illness.
Nutritional supplements seemed to have contributed little or nothing to maintaining physical activity capabilities. In fact, the opposite, a negative effect on physical activity was suggested. This is a perfect opportunity to draw no conclusions until more responses are obtained.
Clearly, presenting an average of 50% of usual physical activity for the overall group of 100 respondents at this point in the review, is thought provoking. At first pass, normal physical activity levels depend on intact cardiovascular and respiratory systems, functioning in concert. But the end-organs of all that oxygen and nutrient delivery are the muscles, brain, and other tissues and organs working in a synergy that we referred to or group as "physical activity."
If 50% of these patients had "a serious heart problem," by now, that would be known. Yes, some present a myocarditis (heart cell inflammation) but most of these are severely or critically ill. Or on the Pathologist's table. So rather than being so targetted, even if one adds back the lungs, a much more global effect on the body as a whole is suggested. Pathologists have already provided many findings distributed throughout the body's organs and tissues that are consistent with this finding in our 100 respondents on this date. And their huge number of symptoms early and during this illness, are again consistent with path and clinical findings. Fortunately, and as they responded, they are suffering an illness of moderate severity. (Not very convenient to take a questionnaire when being mechanically ventilated).
"Healthcare," with its ever-creasing tendency towards hyper-specialization, is not often prepared to do anything with such a symptom list but dismiss it. Or one step less ineffective, to focus in on only one or two items from the list. That can quickly lead to trouble, and on both sides of the exam table.
Targetting each area of organ (or tissue) involvement with specific diagnostic tests to prove presence or absence, and specific therapies aimed at curing or at least improving abnormal findings, sounds like a daunting task and certainly is!
So one must not forget in this less than perfectly clear clinical setting, that with time and basic support, the body tends toward healing itself. Unless a body has strayed so far, through illness or habits, from Walter B. Cannon's "homeostasis" or middle of the road, it usually finds its way back.
Anyone suffering with this illness should find much hope in that.
<<<<<<< Questionnaire answers - start here
(this is where several previous "Lessons" are posted).
This was Lesson 8: How much does "Long-term" COVID-19 impact one's usual activity level?
<<<<<<< Introduction to the Questionnaire
<<<<<<<<< Take the Questionnaire
<<<<<<<<<<< Home page
Lesson 7: It's Physical. It's Emotional. It's Both.
But how much of each?
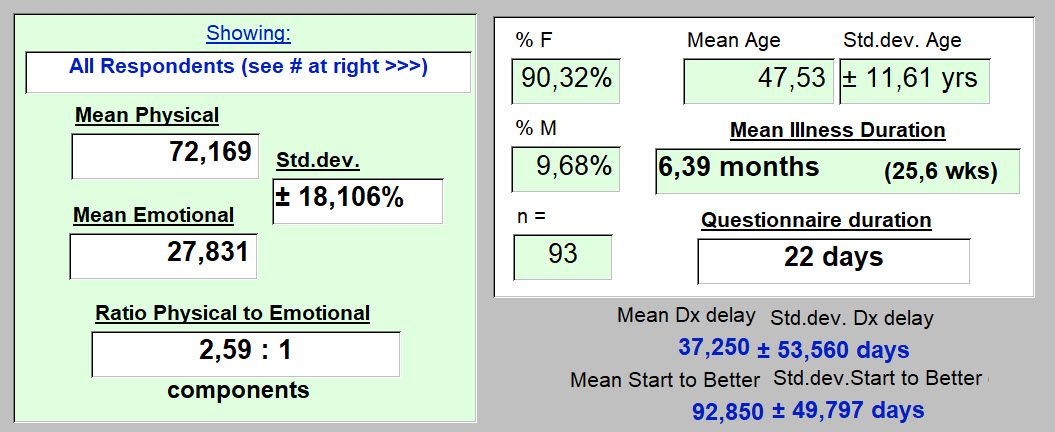
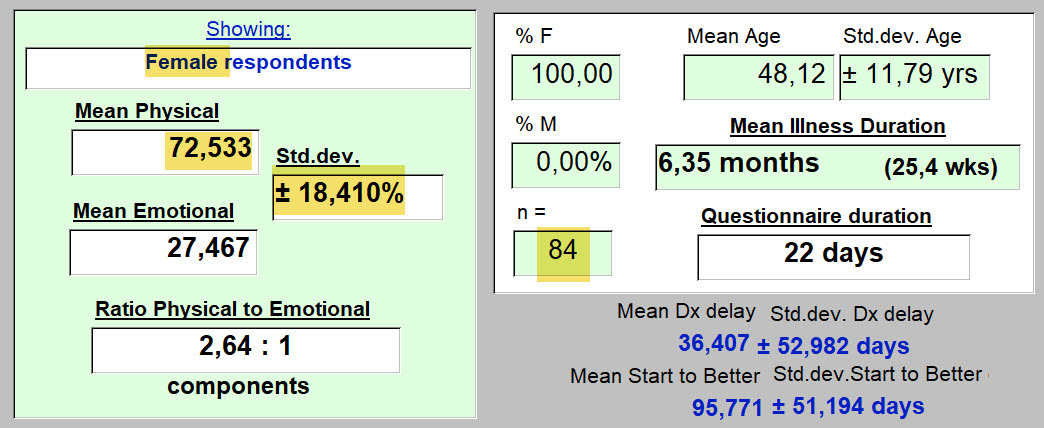
Overall, for 95 kind individuals who responded, the results look like this...
Let's look first at how the question was asked.
Q43 : "There is no illness of the body, that is without emotional, mental, spiritual components. And if one has a reason to become depressed or anxious, our body reacts. It is a unified system. Some days, some parts are more broken than others and that varies from one day to the next. How would you describe the balance of those components in you today? Where are you focused ?"
Possible answers offered:
-
-
-
-
-
- 100% physical & 0% emotional
- 80% physical & 20% emotional
- 50% physical & 50% emotional
- 20% physical & 80% emotional
- 0% physical & 100% emotional
- Don't know. Can't tell.
-
-
-
-
95 people answered so far.
Typical of all questionnaires, a few just didn't understand, are internally inconsistent (like with impossible dates [this illness probably did not start before the respondent was born] ), or whatever. In this case, they (2) get thrown out, leaving 93. So for this question, their answers were excluded. One had responded "80:20" and the other, "50:50." Below, these have been subtracted.
Here's how these 93 replied:
-
-
-
-
-
- 11 (11.83%) chose "Didn't know. Can't tell.
- No one chose "0% physical & 100% emotional" - 0 (0%)
- 1 (1.08%) chose "20% physical & 80% emotional"
- 27 (29.0%) chose "50% physical & 50% emotional"
- 43 (46.2%) chose "80% physical & 20% emotional"
- 11 (11.8%) chose "100% physical & 0% emotional"
-
-
-
-
So the majority elected to respond that "Long-term" COVID-19 is an illness where what is "broken" (to use the term as presented in the question) is "80% physical & 20% emotional."
But the next most frequent response (50:50) was often selected as well.
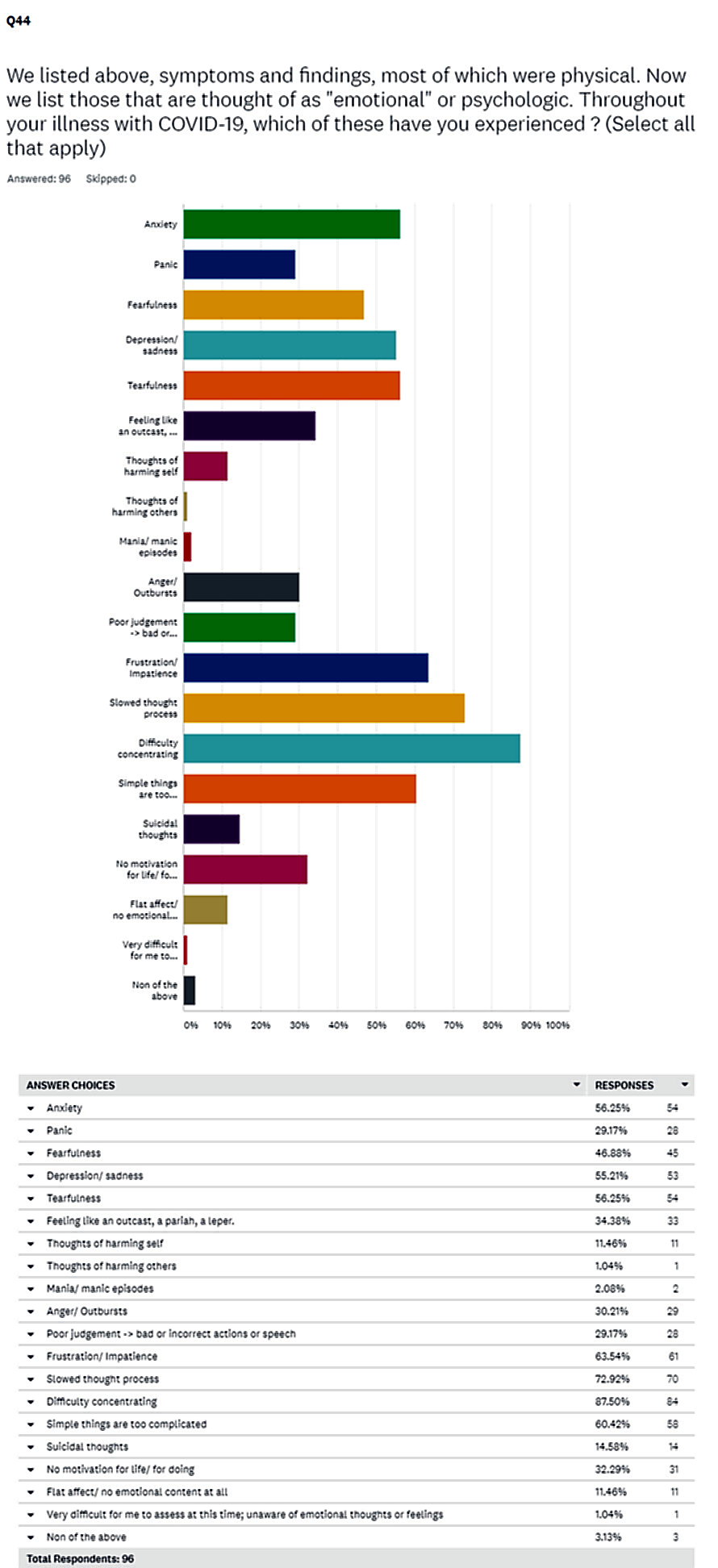
So we need a mean value to summarize with. An average value to represent what those with "Long-term" COVID-19 are living with. And have been living with for about 26 weeks. And here it is.
So to walk you through these results (if needed) : We are here commenting on the responses of individuals who present with "Long-term" COVID-19. This result is not earth-shattering news.
But it gives one, at least I hope so, a meaningful starting point that can be thought of as probably representative.
It should help reduce (or even challenge), "hunches" that we might have about this physical:emotional balance point.
-
-
-
- Reponses so far had been obtained by the 22nd day of the questionnaires use.
- 90% are women. Average age: 47.5 yrs. Then have been ill 6.4 months on average.
- On average, they feel that what is "broken" due to this illness that most (data not shown here) are still living with ... is 72% physical, and 28% emotional. That's what they think.
- The variability in the actual responses, as presented above, before this graphic, generates a standard deviation here of 18.1%. Not into statistics? Don't worry about it. It just means that not everyone chose the same response. We knew that. It's utility will reappear when comparing subgroups. For instance, gender differences. For instance, smokers and non-smokers.
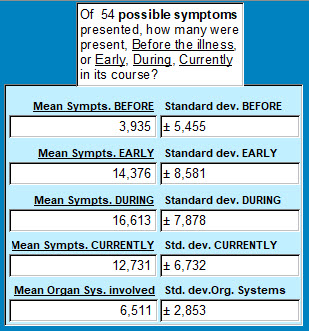
- That "Ratio Physical to Emotional" value above on the left, is also useful for summarizing these results. For each emotional symptom present, on average there are 2.6 physical symptoms. Were there many of both? Yes. A huge (that's not an exaggeration) number of physical symptoms selected in that question (presented elsewhere), and at various times. As I write this, these 93 respondents had the following number of physical symptoms at the times indicated below. And yes, that is a huge number to be experiencing. Even if all are not severe. Imagine, 17 different things bothering you physically throughout your day. And these respondnets were still kind and courageous enough to get it together for 30 minutes and answer the questionnaire! Thank you! :
-
-
So what about that 27.8% of "broken" things being "emotional or psychologic."
The responses today look like this.
These are the psychologic findings that respondents have been experiencing, and living with, captured in a different question of this questionnaire and copied below:
Though the image is blurry, one can make out that only 3 (3.13%) respondents replied "None of the above" to this question.
That leaves us with 19 different psychologic symptoms! And among these: Anxiety, fear, depression/ sadness, tearfullness, feeling like an outcast, frustration/ impatience. It has gone on long enough, and at a level of importance, that now slowed thoughts, difficulty concentrating, and others, make even simple things too complicated.
These people are beginning to suffer from shell shock! Not only would they benefit from a big hug! ... they need professional help to address these outcries for help. It's just that simple. If it's not that simple, it should be.
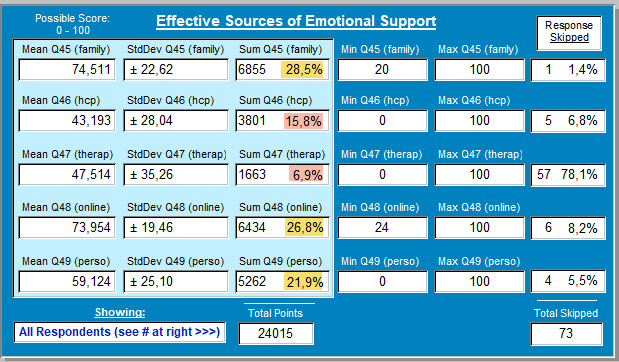
Are they getting help? And from where?
Questions 45, 46, 47, 48, 49 help to answer that. On this date of 4 October:
Just concentrate on the highlighted percentages ...
-
-
-
- Family - is the primary source of emotional support. While that is understandable, and even commendable and reassuting, I hope that some of those families include members who are professionally capable of dealing with the large list presented above of the "broken" emotional pieces.
- The people that the "healthcare system" teaches are there for such emergencies: one's healthcare providers or a separate therapist. These fo not garner many points for effectiveness in addressing the challenge (15.8 & 6.9% of the scores awarded). 78% skippped the "therapist" question. As you read this, if you are thinking: "But who's going to pay for that?" it means the system is broken. Go find yourself a shaman.
- So instead, these respondents turn to online groups and communication. Healing by electrons. Not knocking that at all. But it has moved into position 2 after Family. What has happened to "healthcare"? And how can we fix that?
- And personal strengths and habits have now also outpaced "healthcare" for fixing what is broken. One can only hope that personal resilience (a question covered elsewhere) remains strong. Some have more than others as discovered at the above link.
-
-
Gender differences?
Here are the women ...
Since they are in the majority for this illness, the results are almost identical to the overall results.
How about the men?
Results :
-
-
-
- Do men with "Long-term" COVID-19 illness seem to find more emotional parts that are "broken," than the women?
- For each emotional issue, there are 2.2 physcal ones. And for women that was 2.64 physical problems for each emotional finding.
- CONCLUSION: the emotional components of this illness are more present in men than women. That would be good to anticipate if one gets this illness, and one is male.
- Surprised?
- Why are you surprised?
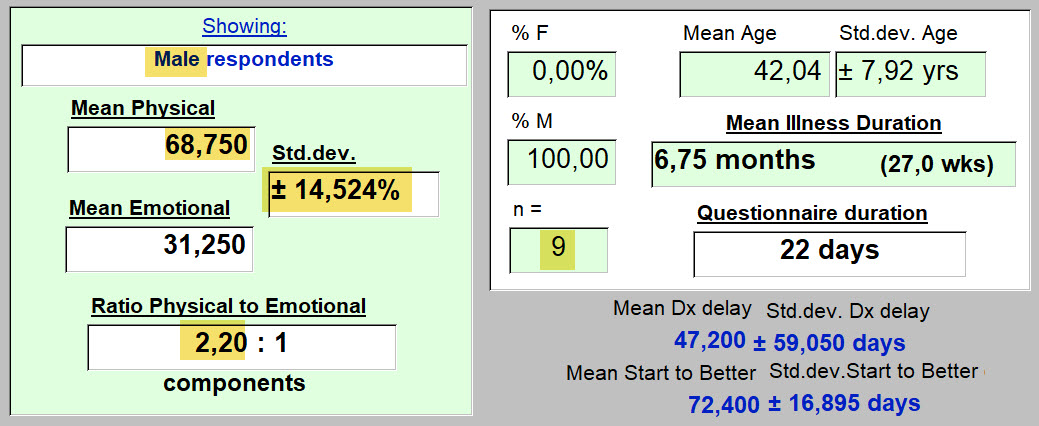
- But, ... are these apparent differences, "statistically significant?" - an important question. (Even if it's response and the question itself, bore you to tears). We don't want to be spreading around our hypothesis that men and women have a different balance of physical : emotional response to this illness, Not unless it's very likely to be true. Let's see...
-
-
Need help!?
-
-
-
-
- The above teaches that there is no significant difference in these mean values based on gender alone.
- Our hypothesis that there actually is a difference, has 55 chances out of 100 of being wrong.
- What might we do if its actually true, and there is a difference, but we can't find it?
- Get more respondents. Only 9 male respondents when this was written (a few more since) isn't much. Maybe we need at least 100. There, you can help by spreading around a link to the questionnaire for those you know with "Long-term" COVID-19.
- More importantly. How nice to have a tool that can tell us when our impressions, based on results right under our nose(s), are dead wrong. Or even sometimes, right.
- Or even better, when they teach us something we hadn't seen at all, or hadn't even imagined. Then it's worth the effort. Then, as said one day in Arkansas: "Even a blind hog finds an acorn, every now and then."
-
-
-
Sometimes questionnaire responses generate results that are certainly real, but for which an answer is not immediately apparent. Sometimes information from another question in our survey, can be used to better understand. To shed light as well as heat. Here's an example:
Smoking
Here are responses to Question 12, about smoking history of respondents. This particular respondent has a smoking history of 21 to 40 pack-years.
51% are Non-Smokers. 46% smoked in the past or still do.
In the UK, 14.7% of the population smokes. USA 13.7% of the population smokes, as seen above.
So there already a question is forming. There are more smokers in this sample of the population that presents with "Long-term" COVID-19, than in the population.
As a past Professor of Neuroanatomy used to say: "Why? ... We do not know."
Next
Do Non-smokers and those with a Smoking History experience a different balance of Physical and Emotional "brokenness"?
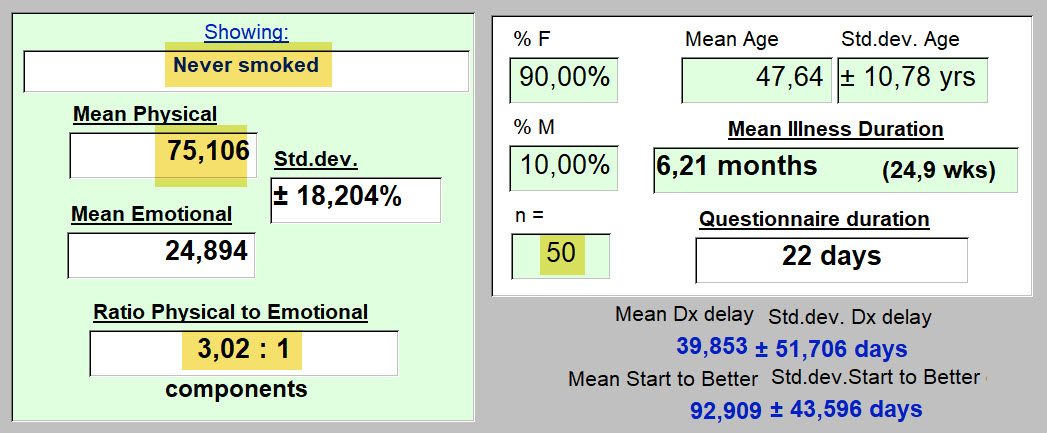
First, the Non-Smokers:
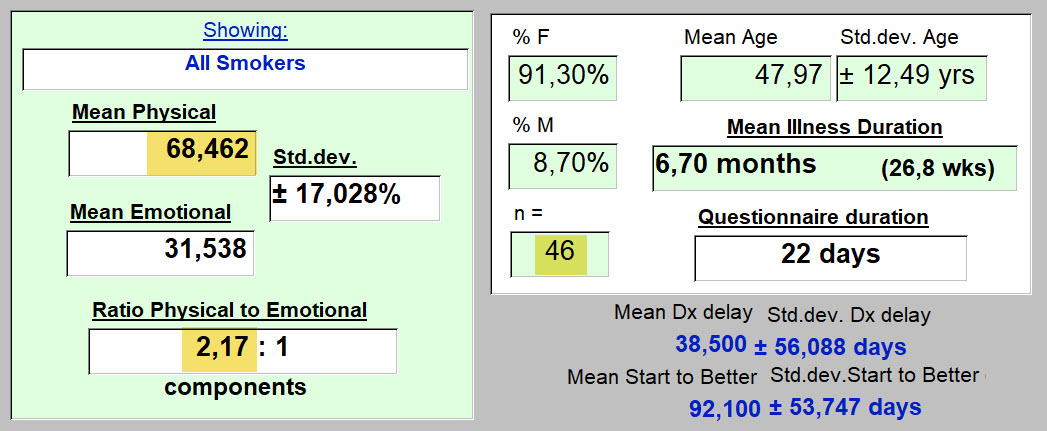
Next, the Smokers
Interpretation :
-
-
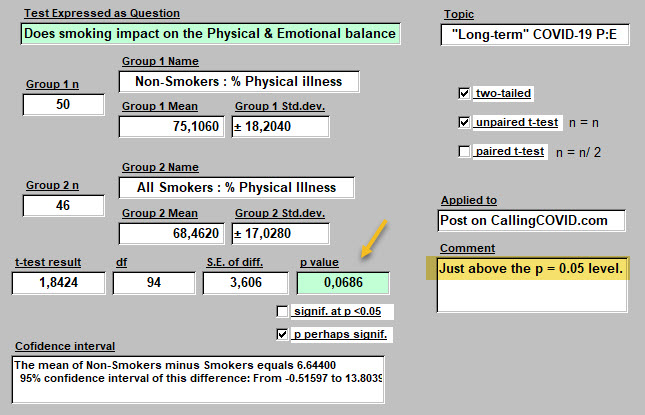
- Those who do not smoke, have a different balance of Physical and Emotional symptoms than do smokers. Non-smokers have on average 75% Physical Symptoms and 25% Emotional. Smokers, 68.5% Physical and 31.5% Emotional. Some would say: "Pretty close." As more responses come in, we'll see how this result changes.
- But perhaps we already have enough responses to hint at an answer. To be robust enough to tolerate a statistical onslaught.
- And if their is a difference an appropriate answer may still be: "Why? We do not know ..."
- Is this suggested difference in mean % Physical values real? Here comes the test ...
-
The difference generates a p value of about 0.07. That means there are about 7 chances in 100 that the apparent difference discovered in Smokers compared with Non-Smokers in the mean %Physical to % Emotional Balance is not real and arose by chance. Since 7 out of 100 is not much chance, I'd bet on our hypothesis that Smokers and Non-Smokers live this illness slightly differently.
To see if this holds, a few more responses would help to confirm that this subtle difference is real.
Why would this be? What has smoking done to change this rapport? "Why? ... we do not know."
So what's the point?
-
-
- That all those suffering with this illness are not perfectly alike.
- That personal habits acquired before becoming infected are today playing a role in recovery.
- Notice that no difference was seen in duration of illness, delay of diagnosis, nor in number of days from start of illness to when starting to feel better.
- That methods exist for finding and confirming actual differences in what, at first glance, looks like a uniform population of "Long-term" COVID-19 sufferers. When looked at a little more carefully, one finds different sub-groups. These add to our understanding of this illness. Even in illness, we are each individuals.
-
CONCLUSIONS
For both women and men with this illness,
-
-
- Physical symptoms can be identified as present
- Emotional symptoms can be identified as present
- Besides gender, other personal habits impact on how Physical and Emotional components of this illness are perceived. (Smoking or not).
- While there is a balance between the two that varies from one person to the next, on average for what this specific illness effects or "breaks" is 72% physical and 28% emotional. Is this different than the response to any other serious illness? But trying to convince oneself that it's all one or the other, is wrong we have seen, and probably won't work. Might delay healing.
- The number of defects or deficits distancing respondents from a desired state of unified health, are usually very numerous for these particular patients (i.e., many physical symptoms reported). Perhaps unusual from what happens most offen in Medicine. (Think of appendicitis, a heart attack, a breast cancer, pulmonary embolism, a broken femur, an itchy rash). This is a multi-system disease. (Reminiscent of a car accident victim who has sustained a multi-trauma set of injuries).
- While some will suggest that a treatment for the physical components of this illness is lacking (several still experimental under clinical study have suggested effectiveness, and vaccines a promise for the future), that is not true for the host of psychologic symptoms that are manifesting each day in these responses.
- And yet, use of available therapies in that domain at a professional level are not being frequently sought, preferring to relie on other sources scored higher as potentally effective for emotional support.
- Most individuals having symptoms of a broken leg (not actually studied here), would not hesitate to seek aide from a source beyond family and friends, to get that painful problem fixed. A whole constellation of painful emotional symptoms were uncovered through this questionnaire. And yet, the hesitation for moving promptly towards professional help is all too evident in the responses. Identifying why is a very essential next step.
- Is effective care in the setting of this exact 72:28 balance of physical and emotional symptoms on this day, being obtained from "healthcare"? If not, what's missing? There are just too many broken souls out there to keep wearing blinders like my horse used to do. Come on my fellow physicians: take off those blinders and see your patient. Perhaps for the first time.
-
Presented again below are quotations from the respondents. These are their responses to the question which is phrased as follows in the questionnaire:
"Time now to listen to you directly. To hear your new found expertise with COVID-19.
If you could offer a few words of advice to those from whom you sought care during this illness, what would you say?"
Here is what some wrote ...
(75 responded, 21 skipped this opportunity to write any thoughts, as of Oct. 4, 2020).
Where would the following thoughts have come from?
I have to assume, from what they experienced and were made to feel in their exchanges with "the System."
These have not been subselected for effect. Some convey a positive response to exchanges with "healthcare." Most do not.
--------
"Listen and don’t dismiss."
"This is not just anxiety, its not all in our head, we are suffering, hundreds of thousands of us who never got better. Do your jobs and help us instead of accusing us of being crazy hypochondriacs!"
"Listen, try to understand and show empathy. If you are not an expert, refer to someone who may be! It's ok not to have the answers but don't be dismissive."
"Believe me, be sympathetic, refer me to specialists."
"Keep researching, keep looking for answer and be honest and transparent where you don't know. I wouldn't be seeking your help if I wasn't suffering."
"LISTEN to your patient, and BELIEVE them."
"Try to understand what the illness is like for me."
"I have very few words. I lost all faith in providers after this experience. The total lack of care, compassion, and guidance of the doctors was traumatic in itself."
"See us face to face and perform tests to find out what is going on in our body rather than playing guessing games."
"Medical profession need to be up to speed with long Covid."
"Please take time to read the newest studies, research, and articles written by those struggling. We don’t expect you to have the answers but we do expect you to listen, believe, educate yourself and advocate for us."
"Thank you to those who believed me - particularly my close family and my doctor, and therapists I have sought help from."
"... just listen, were not mad!"
"Listen more. Seek answers, it's what we who suffer need in order to improve. We won't all "get better in time", some have physical ailments as a result of the virus."
"Be patient."
"Don't put everything down to anxiety."
"Listen to the patient. You may have concerns for their breathing but other symptoms are also worrying for us. Those other symptoms may also point in a direction you hadn’t considered especially if tests come in normal."
"Listen to your patient as they know how they feel. Support the patient even if there isn't any treatment."
"Admit you dont know but continue to learn."
"Be open-no preconceived boxes for symptoms and treatments."
"Please believe your patients, and let them know you believe them, - show empathy even if you don’t understand how one virus can cause such a toll or wide range of symptoms."
"Remember it could be you."
"Listen, empathy, believe us."
"You didn’t know enough. I don’t blame you for that. But you didn’t try hard enough to learn from emerging sources. I blame you for that. You were overworked. I don’t blame you for that. You didn’t make sure I was checked on and you left my loved ones to support me on their own. I blame you for that. You made light of my suffering. That hurt. I will never trust the NHS again. I will do everything I can to never have to talk to healthcare professionals for the rest of my life."
"...slow down and LISTEN and look."
"Listen to us. Do more."
"Believe, listen, offer tests to exclude other issues, reassure even if all tests show nothing, that this is real. Advise to rest and convalesce."
"Listen, believe, Learn, care, respect and keep in touch even if you cannot do much."
" keep up the good work "
"Keep listening to the patients. We will be the ones giving you answers for a better research and care."
"Empathy goes a long way, especially if it is phone consultation. It would have been helpful if doctors had checked in on me, rather than me doing it once a month when my sick note ran out. It was hard to speak to 12+ doctors over the past 5 months, a consistent doctor/small group of doctors if more practicable would have been better."
"Listen to your patients, give them at least the allotted time, read the research and leave no stone unturned. Remember your clinical judgement rather than putting so much weight on lab tests and assess new symptoms as you would without Covid."
"Be open minded and keep looking for answers."
"You needed to listen and be much more supportive and understanding."
"Listen to symptoms, focus on clinical experience and use the two to find creative care solutions."
"I am very very lucky to have access to excellent medical care, doctors who are researching this virus to better help their patients and I know how rare this is!"
"Should have looked up my medical history/listened /believed me in the beginning."
"... algorithms are useless. You are medically trained for what? To look at a screen and find out about a disease that is too new for systems and bureaucracy. The answers lie with your patients and educating yourselves. Ignore the 'machine and do what you first got into the profession for. Helping people."
"It would have been helpful if you had not just listened, but actually heard when I was saying. To not be so insensitive and judgemental; blaming all my symptoms on being overweight and my mental health. To please try and treat me holistically and not just separating out symptoms. To actually do some reading and a bit of research about long covid and to see that I am not making this up. I wish you had made me feel validated instead of being left sad and frustrated."
"Don't treat us as imagining we are ill, help us."
"I know not any one has answers yet but TRY SOMETHING."
"I mostly have had positive experiences."
"Don't be dismissive of concerns of those who consult you. This includes taking complaints of particular ailments seriously even if they are not present at the time of the consultation."
"Don’t be afraid to say “we don’t know” - that is a sign of intelligence to me. Express you believe what I’m telling you directly to me. I can tell you do, but that affirmation is soothing. Instruct ALL staff to wear masks correctly ALL the time. Most do, but I did encounter a few who wore it below their nose. Please REQUIRE AND ENFORCE requirement on wearing masks. If someone won’t don’t see them. Online support groups are not for everyone, but offer that information to your patients. My PCP puts an update about local Covid stats, what they mean, trends, and updates on clinical studies."
"Be able to say you don't know share resources / talk to other doctors and give your patients that benefit of the doubt no one knows what this thing is quite yet.. Keep your politics out of my health care!"
----------------
As you read through the above, certain responses for advice to healthcare providers may have caught your attention more than others. You may even have found a favorite.
Mine is: "Remember it could be you."
And that, because it's quite true.
----------
This has been Lesson 7: It's Physical, It's Emotional. It's Both.
Here is a link back to the previous lessons emerging from these preliminary results.
An Introduction to the Questionnaire.
<<<<<<<< Home
BIO: Principle Investigator
The creator and moderator of this website welcomes you.
Here's the SHORT VERSION of his BIO:
He is a retired General Surgeon and ICU Director who has published his work in the peer-reviewed literature pertinent to his domain. At present his interests include both pursuing a scientific understanding of an illness currently referred to as "Long-term" COVID-19, and at the same time, evaluating the effectiveness of intentional healing of this illness at a distance. That occupies at present, his days and much of his nights.
For more information, you will have to bite the bullet, and read the LONG VERSION.
----------
LONG VERSION of his BIO
Born in Belgium in 1950 of parents who met during WW-II, I lived most of my life in the United States, with occasional returns to Belgium and a few years spent in Cambodia in my youth.
I returned to Belgium in 2001 to care for family, and have lived here to the present.
A graduate of Tulane University with studies in English and French Literature, Art History, Theatre, I participated in many activities in the university’s Music Department and throughout the city.
After spending some time working on the island of Guam, I returned to the Washington, DC area, and continued musical studies while working in local hospitals, taking science courses, and conducting Genetics Research.
I entered Medical School at the George Washington University Medical Center in 1980.
After graduating with a Doctor of Medicine Degree, I was accepted into Surgical Residency which I completed in 1986. During those years, Surgical Research was a large part of my activities while acquiring clinical skills across the surgical subspecialties. Research projects included developing techniques for pancreatic islet cell separation and auto-transplantation, defining the presence of extra-thyroidal calcitonin, and pursuing its origins from the pulmonary neuroendocrine cell, then extending this work to define the role of extrathyroidal calcitonin in patients with large burns, and inhalational injuries. Published findings at that time continue to influence further published research today, and specifically procalcitonin’s role in pulmonary illnesses, including the present COVID-19 clinical setting.
For 18 months after completing training, I worked in a small hospital’s Emergency Department (Warrenton, VA), working 24 hour shifts, as the only physician directing and managing the care of an average of 114 patients per day. Once the hospital where I wanted to establish my practice had been built, I began a private practice of General Surgery at several hospitals in Northern Virginia, also serving several years as ICU Director in one of these. That position was accompanied by the early development of a Quality ICU database system in which all patients were entered and studied, contributing to improved patient outcomes, and feedback for those providing care. I served at that time as Director of the Trauma Service at the same hospital. Early use of fine needle aspiration (FNA) and immediate cytology was also implemented during this period, simplifying the management of breast and thyroid masses, and other disease states presenting with a mass, in clinical practice.
In January 2000 these activities were interrupted to devote more attention to family members who had become ill. Eventually, during 2001, a transition was effected to bring members of my family back to where they had begun their lives in eastern Belgium. I also assumed the care of a handicapped cousin, continuing end of life care for these until these challenging needs had come to an end. Given the unfortunate evolutions in private practice that I had lived through, along with other professionals in the United States leading up to that time (late 1990’s), I elected to stay in my family’s small town in Belgium, even after family needs had become less pressing, rather than returning to the United States.
While here, my primary activity growing out of prior studies and training was related to an in-depth study of 1,25 hydroxycholecalciferol (Vit-D) in the population around me, and presenting results through presentations made locally at the Clinique du Soleil, which I began 10 years ago. The goal was to counter the high frequency of deficient serum Vit-D levels in populations where I now reside. An additional activity that grew out of that interest, was the case study of individuals meeting clinical criteria for the newly accepted diagnosis in the DSM-5, of Prolonged Grief Disorder after the death of a loved one.
This psychosocial research in collaboration with Holly G. Prigerson, PhD of Harvard and the Weil Cornell School of Medicine, involves applying her work through French translations and application to patient care here in Belgium.
Presentation of such case reports, the last one scheduled for Utrecht, Holland last March, were interrupted by the appearance of the present viral pandemic.
An additional ongoing project involves the development of a protocol for the use of Red and Near-Infrared wavelenghts in a critical care setting for those with pulmonary involvement with COVID-19.
The continued attraction for a scientific approach to problems arising out of the worldwide infestation with the SARS-CoV-2 virus has sustained new activities in spite of more limited displacements. Studying those currently referred to as the “long-term” COVID-19 presentation of this illness, is ongoing. Initial inroads towards understanding this rather atypical viral illness are being made with a detailed questionnaire. This tool has already received enough response to generate much interest personally and additionally from others located at a distance. Currently, this survey device will soon be extended to populations typically thought of as less well served, and with already documented worse outcomes from the COVID-19 illness. In so doing, collaboration with other researchers located around our world, has been initiated, and this should extend significantly the knowledge obtained on this and other topics that will likely emerge.
At the same time, a portion of available time and effort is dedicated to pursuing a deeper understanding of intentional healing at a distance. That topic is introduced and expanded upon elsewhere on this site. While such an undertaking may be viewed by some as unscientific, and quickly glossed over, that may be a myopic view of science and its boundaries. At times when science doesn’t seem to fit or to know, one can correctly add without concern, that science doesn’t know yet. So this study is also being pursued simultaneously, and with whatever tools can contribute to its badly needed success at this time.
In pursuing current interests, I am not the employee of any orgaization, nor sect, nor affilitaed with any organized religious group nor teaching institution. How results will be shared has already been commented on elsewhere. Where patients can benefit from sharing my study results I will be in favor of implementing that. While I have in years past participated in contributing to the peer-reviewed literature in my disciplines, that should not be the only, nor is it always the best, method of getting what has been learned to those who can benefit. I have collaborated with those who have successfully pursued as a goal, a quite extensive peer-reviewed bibliography in their CV. That was never a personal goal. That choice has not kept me from providing compassionate and effective care to many patients during many years. When elected by my peers to one position or another in the past, good outcomes and low complication rates were I believe, the primary motivators for such votes of confidence.
Professionally for years I have expressed the central goal of my practice as follows: to relieve suffering, and heal the sick where possible. All of the above activities would seem to have direct ties.
So some things never change.
<<<<< Back to the Questionnaire Introduction page
Lesson 6: Impact of "Long-term" COVID-19 on Quality of Life perceptions
It makes sense that being sick doesn't feel good.
It makes sense that although many things contribute to one's Quality of Life (QoL), losing one's health may quickly make those other things seem less important contributors.
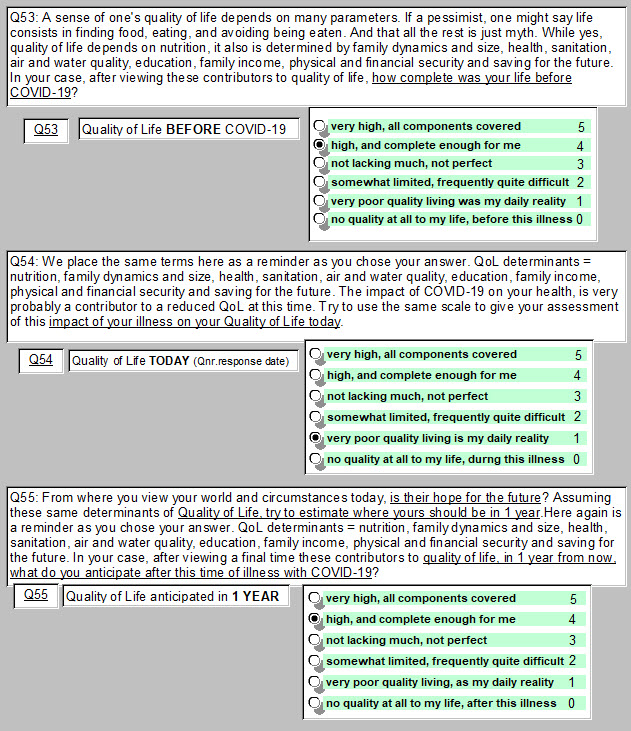
We asked about their perceptions of Quality of Life from those who identify as "Long-term" COVID-19 patients. How did they view QoL BEFORE becoming ill? How about DURING the illness as they responded to a questionnaire? And how would they project their Quality of Life at 1 YEAR into the future?
Here are the questions asked :
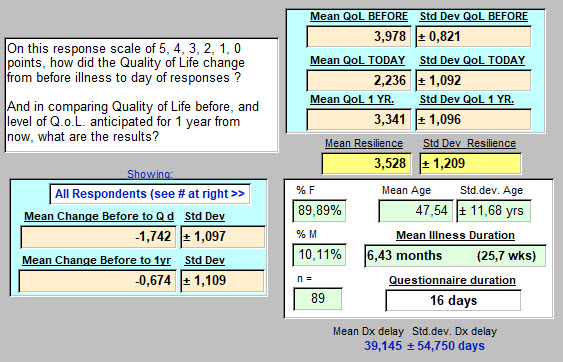
- The answers provided were summarized on September 28th, with 89 respondents.
- Above are also shown one person's responses.
- Response options were scored from a maximum QoL of 5, to no QoL at 0, and as shown. This permitted subsequent quantitative summary and analysis. These are referred to below as QALYs or quality points.
- It may not seem that a change from 4 to 1 QALYs is a large change. Yet it probably is. For instance: 4, QoL "high, and complete enough for me," to 1, QoL "very poor quality living, as my daily reality." That is clearly a major change in the quality aspects of that persons existence.
- Only the phrased responses, without numbers, were shown to respondents as they answered.
- Responses were obtained at a single time, and not at the three times requested through the 3 questions. (Before, During, in 1 Year). So responses for Before & I Year are based on recall of the past (6 months ago), and projection or anticipation of the future (at 1 year).
--------
And here are the results on September 28th:
We'll walk you through these responses below ...
-
-
- 89 respondents, 90% female and with an average age of 47.5 years (range: 17 to 72.3)
- Illness duration was 6.4 months on average.
- The interval from when they became ill, to when they were diagnosed with this illness (not all were), averaged 39.1 days, with a large variation as seen above.
- On this 0 to 5 Likert scale, BEFORE becoming ill, the mean value is 3.978±0.821 QALYs.
- On the day of response, DURING the illness for most, the mean is 2.236±1.092 QALYs.
- Projected 1 YR in the future, respondents answers generate a mean of 3.341±1.096 QALYs.
- On the left above, from BEFORE to DURING this illness, -1.742±1.097 QALY points lost.
- From BEFORE this illness to 1 YR in the future, a mean of -0.674±1.109 QALY points lost.
-
Analysis of Results:
Some readers may simply "eyeball" the results and move towards an interpretation.
Comparison of several of these mean values may be of use. Possibly adding confirmation to impresseion.
-
-
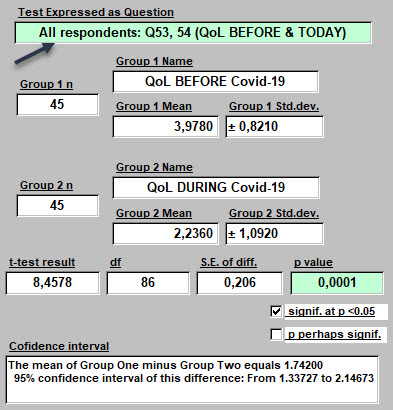
- These are results of Student's t-test, paired, since both responses come from the same respondent (i.e., not comparing males with females, but two answers from the same person). That is why the n value of 89 respondents became 45 as seen above when challenging these means with Student's test.
- The loss of Quality of Life from BEFORE to DURING this illness was very significant.
- With a p value = 0.0001 that suggests that there is only 1 chance in 10 000, that this hypothesis of a loss of quality in life is false. It's probably true.
- With 95% confidence, that amount of loss of quality in life due to this illness, varied from 1.3 to 2.2 QALYs for these respondents.
-
Interpretation:
-
-
- This may be a confirmation of suspicions for some, but not a surprise.
- "Long-term" COVID-19 is a major illness: lasting a very long time, and with many symptoms reported (see other article). At time of response, these respondents reported a mean of 15.4±7.8 symptoms. (And yet, they still responded! Thank you! )
- So a loss of up to 2 steps down in Quality of Life, and as confirmed statistically here, is a major loss. Seemingly undeniable.
-
But we can never get back to the past exactly as it was. And perhaps shouldn't try.
But if one liked one's Past Quality of Life, as sensed overall and combined into a single answer here,
most would assume that after this illness has passed and one has recovered, that previous QoL could also be recovered.
Is that the case? Do those with "Long-term" COVID-19 anticipate a full return to quality?
From the result presented at the top of this page, it may not be so.
We are not trying to predict the future here.
We are simply presenting how these respondents feel today, about possibilities.
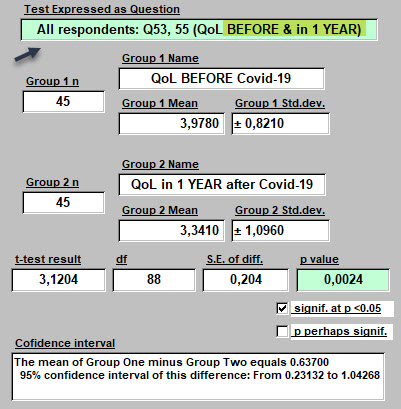
Here is the Analysis of those Results: BEFORE compared with in 1 YR
These are of course, the same 89 respondents.
-
-
- Comparing means for Quality of Life BEFORE, and in 1 YEAR, respondents anticipate losing a mean of -0.674±1.109 QALYs.
- With 95% confidence, that ranges from 0.23 to 1.04 QALYs.
- How certain is that? That the anticipated future, will have less Quality of Life, than did life lived before COVID-19?
- The p value is 0.0024. Statisticians would say the difference in these mean values is significant because it's below 0.05. Another way of saying it is that there are only 24 chances out of 10 000, (ten thousand) that this apparent difference is not real, not present.
- Again, we are not predicting the future here, or trying to. We are trying to add clarity to better understand the future anticipated today, by respondents. This answer obtained at a mean of 25.7 weeks into this illness.
-
Interpretation:
-
-
- Clearly, less Quality of Life is anticipated for the future, when compared with known QoL in the past.
- While some answered that there would be no change in past and future life quality. 7 responded a level 5 QALY Before and in 1 YR. And 21 responded a level 4 QALY Before and in 1 YR. No one suggested life would be improved by this illness.
-
COMMENT
And yet, some would suggest that for some, things may be better than they were. Not worse.
- Other comparisons could be made and will be in subsequent articles: gender differences in perceiving Quality of Life, for example. Enough has been presented here to think about.
- How does one anticipate a cheerier future? One hopes for it. And how we hope, if done successfully, is not just done willy-nilly. There can be a method. Often unconscious perhaps. At times, intentionally pursued and learned. At times, supported by someone else.
- So can we translate the above result (and it seems pretty certain) into some degree of hopelessness for the average respondent to these three questions?
- If so, that may be a place to start now, today, to make inroads into helping to boost hopefullness. Yes, even while still feeling crummy.
- There are experts in this pursuit. I am not one. Not because I am not hopeful personally for the future Quality of my Life and that of others. I am.
- But there is a path to follow on that walk from hopelessness to filled with hope. And sometimes, taking a beating in life, may ultimately lead to being even more filled with hope than we were before the hard times arrived. Sounds a bit like Post Traumatic Stress Disorder (PTSD).
Heading in that positive direction, might just start here. With a review of some experts in this.
-----------
This was Lesson 6.
Here are those that came before, also grown from the seeds of these terrific responses, if you missed them: (those that are indented, are more recent, and therefore have more data. But don't miss what came before! ).
Lesson 1: Test results - how uncertainty changes our lives
Lesson 1a: Test results - adding light as well as heat. A concise reporting of test results. (at 77 respondents on that date).
Lesson 2: So what about that weight gain?
Lesson 2a: More responses = more insights on WEIGHT
Lesson 3: Effective emotional support - where shall we turn?
Lesson 4: "Long-term" COVID-19 - How scary is that?
Lesson 5: Fostering Resilience
<<<<<<<<< Introduction to the Questionnaire
Direct link to the questionnaire >>>>>>>>>