Lesson 7: It's Physical. It's Emotional. It's Both.
But how much of each?
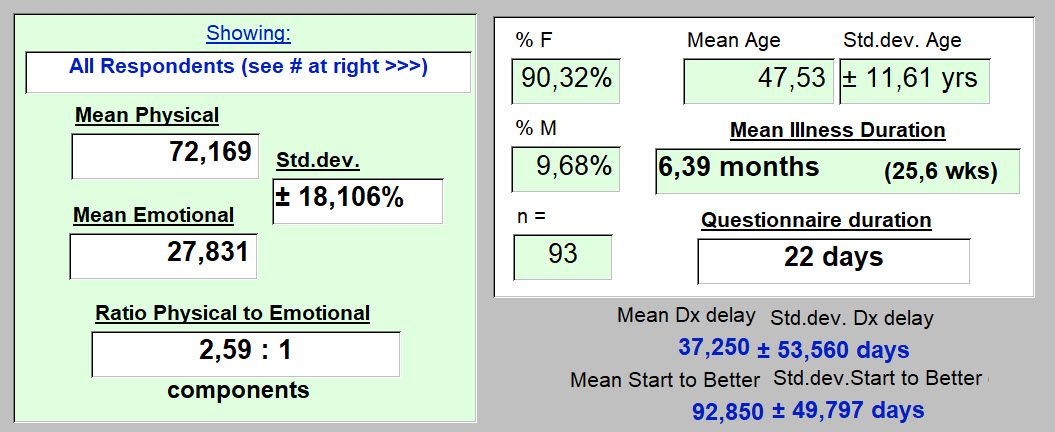
Overall, for 95 kind individuals who responded, the results look like this...
Let's look first at how the question was asked.
Q43 : "There is no illness of the body, that is without emotional, mental, spiritual components. And if one has a reason to become depressed or anxious, our body reacts. It is a unified system. Some days, some parts are more broken than others and that varies from one day to the next. How would you describe the balance of those components in you today? Where are you focused ?"
Possible answers offered:
-
-
-
-
-
- 100% physical & 0% emotional
- 80% physical & 20% emotional
- 50% physical & 50% emotional
- 20% physical & 80% emotional
- 0% physical & 100% emotional
- Don't know. Can't tell.
-
-
-
-
95 people answered so far.
Typical of all questionnaires, a few just didn't understand, are internally inconsistent (like with impossible dates [this illness probably did not start before the respondent was born] ), or whatever. In this case, they (2) get thrown out, leaving 93. So for this question, their answers were excluded. One had responded "80:20" and the other, "50:50." Below, these have been subtracted.
Here's how these 93 replied:
-
-
-
-
-
- 11 (11.83%) chose "Didn't know. Can't tell.
- No one chose "0% physical & 100% emotional" - 0 (0%)
- 1 (1.08%) chose "20% physical & 80% emotional"
- 27 (29.0%) chose "50% physical & 50% emotional"
- 43 (46.2%) chose "80% physical & 20% emotional"
- 11 (11.8%) chose "100% physical & 0% emotional"
-
-
-
-
So the majority elected to respond that "Long-term" COVID-19 is an illness where what is "broken" (to use the term as presented in the question) is "80% physical & 20% emotional."
But the next most frequent response (50:50) was often selected as well.
So we need a mean value to summarize with. An average value to represent what those with "Long-term" COVID-19 are living with. And have been living with for about 26 weeks. And here it is.
So to walk you through these results (if needed) : We are here commenting on the responses of individuals who present with "Long-term" COVID-19. This result is not earth-shattering news.
But it gives one, at least I hope so, a meaningful starting point that can be thought of as probably representative.
It should help reduce (or even challenge), "hunches" that we might have about this physical:emotional balance point.
-
-
-
- Reponses so far had been obtained by the 22nd day of the questionnaires use.
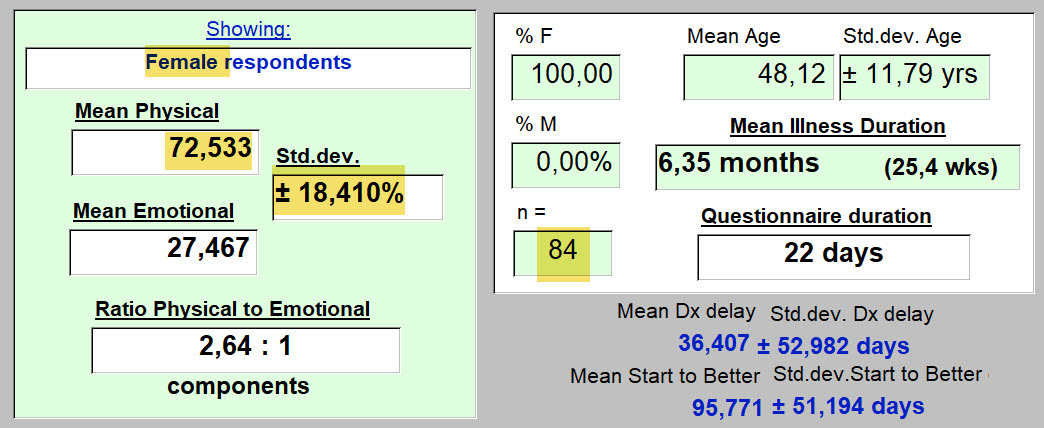
- 90% are women. Average age: 47.5 yrs. Then have been ill 6.4 months on average.
- On average, they feel that what is "broken" due to this illness that most (data not shown here) are still living with ... is 72% physical, and 28% emotional. That's what they think.
- The variability in the actual responses, as presented above, before this graphic, generates a standard deviation here of 18.1%. Not into statistics? Don't worry about it. It just means that not everyone chose the same response. We knew that. It's utility will reappear when comparing subgroups. For instance, gender differences. For instance, smokers and non-smokers.
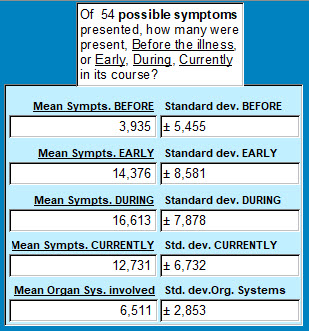
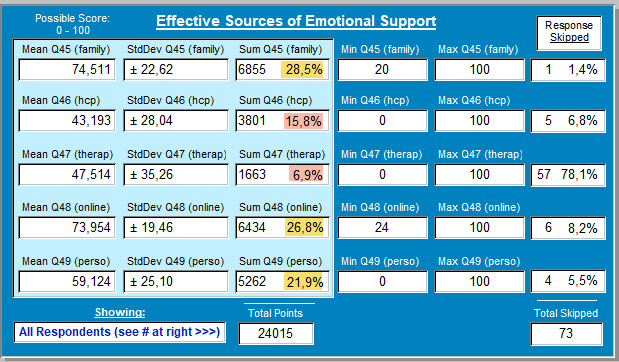
- That "Ratio Physical to Emotional" value above on the left, is also useful for summarizing these results. For each emotional symptom present, on average there are 2.6 physical symptoms. Were there many of both? Yes. A huge (that's not an exaggeration) number of physical symptoms selected in that question (presented elsewhere), and at various times. As I write this, these 93 respondents had the following number of physical symptoms at the times indicated below. And yes, that is a huge number to be experiencing. Even if all are not severe. Imagine, 17 different things bothering you physically throughout your day. And these respondnets were still kind and courageous enough to get it together for 30 minutes and answer the questionnaire! Thank you! :
-
-
So what about that 27.8% of "broken" things being "emotional or psychologic."
The responses today look like this.
These are the psychologic findings that respondents have been experiencing, and living with, captured in a different question of this questionnaire and copied below:
Though the image is blurry, one can make out that only 3 (3.13%) respondents replied "None of the above" to this question.
That leaves us with 19 different psychologic symptoms! And among these: Anxiety, fear, depression/ sadness, tearfullness, feeling like an outcast, frustration/ impatience. It has gone on long enough, and at a level of importance, that now slowed thoughts, difficulty concentrating, and others, make even simple things too complicated.
These people are beginning to suffer from shell shock! Not only would they benefit from a big hug! ... they need professional help to address these outcries for help. It's just that simple. If it's not that simple, it should be.
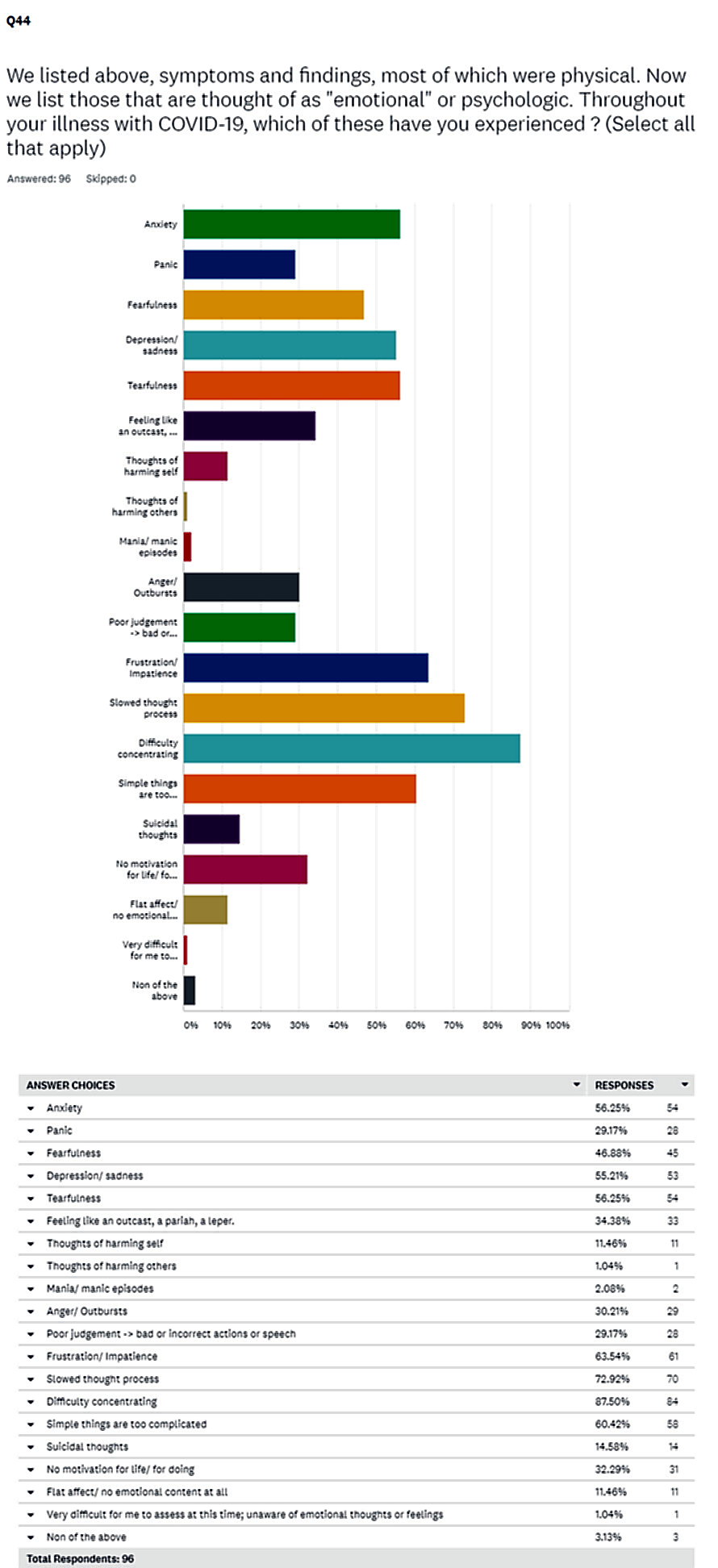
Are they getting help? And from where?
Questions 45, 46, 47, 48, 49 help to answer that. On this date of 4 October:
Just concentrate on the highlighted percentages ...
-
-
-
- Family - is the primary source of emotional support. While that is understandable, and even commendable and reassuting, I hope that some of those families include members who are professionally capable of dealing with the large list presented above of the "broken" emotional pieces.
- The people that the "healthcare system" teaches are there for such emergencies: one's healthcare providers or a separate therapist. These fo not garner many points for effectiveness in addressing the challenge (15.8 & 6.9% of the scores awarded). 78% skippped the "therapist" question. As you read this, if you are thinking: "But who's going to pay for that?" it means the system is broken. Go find yourself a shaman.
- So instead, these respondents turn to online groups and communication. Healing by electrons. Not knocking that at all. But it has moved into position 2 after Family. What has happened to "healthcare"? And how can we fix that?
- And personal strengths and habits have now also outpaced "healthcare" for fixing what is broken. One can only hope that personal resilience (a question covered elsewhere) remains strong. Some have more than others as discovered at the above link.
-
-
Gender differences?
Here are the women ...
Since they are in the majority for this illness, the results are almost identical to the overall results.
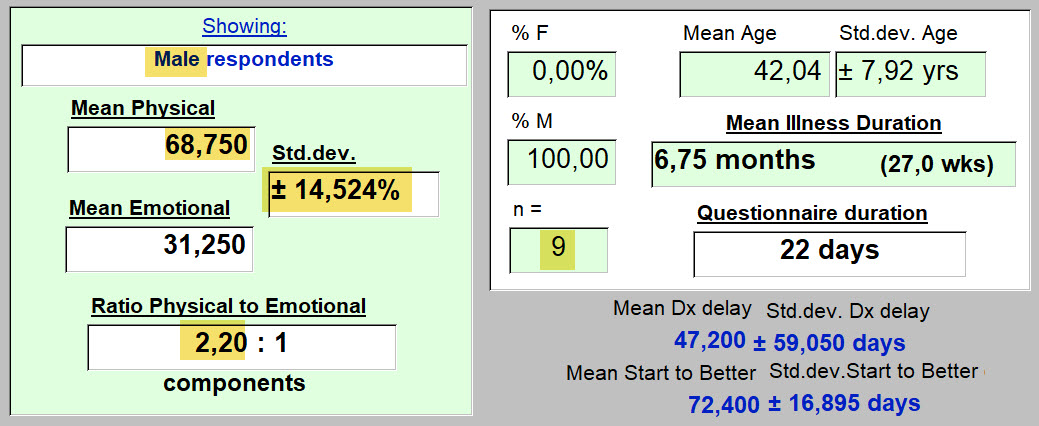
How about the men?
Results :
-
-
-
- Do men with "Long-term" COVID-19 illness seem to find more emotional parts that are "broken," than the women?
- For each emotional issue, there are 2.2 physcal ones. And for women that was 2.64 physical problems for each emotional finding.
- CONCLUSION: the emotional components of this illness are more present in men than women. That would be good to anticipate if one gets this illness, and one is male.
- Surprised?
- Why are you surprised?
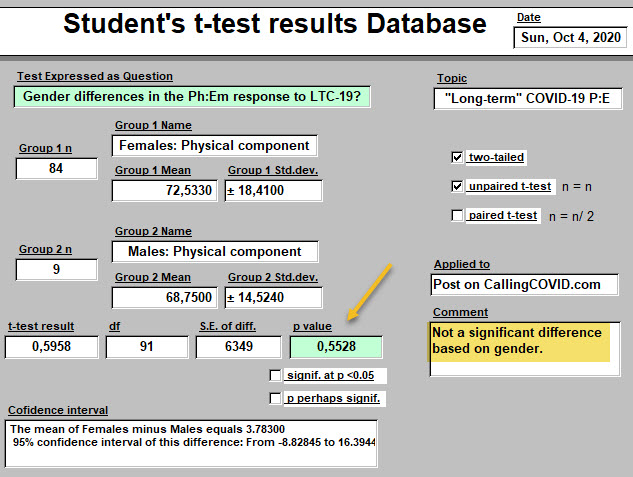
- But, ... are these apparent differences, "statistically significant?" - an important question. (Even if it's response and the question itself, bore you to tears). We don't want to be spreading around our hypothesis that men and women have a different balance of physical : emotional response to this illness, Not unless it's very likely to be true. Let's see...
-
-
Need help!?
-
-
-
-
- The above teaches that there is no significant difference in these mean values based on gender alone.
- Our hypothesis that there actually is a difference, has 55 chances out of 100 of being wrong.
- What might we do if its actually true, and there is a difference, but we can't find it?
- Get more respondents. Only 9 male respondents when this was written (a few more since) isn't much. Maybe we need at least 100. There, you can help by spreading around a link to the questionnaire for those you know with "Long-term" COVID-19.
- More importantly. How nice to have a tool that can tell us when our impressions, based on results right under our nose(s), are dead wrong. Or even sometimes, right.
- Or even better, when they teach us something we hadn't seen at all, or hadn't even imagined. Then it's worth the effort. Then, as said one day in Arkansas: "Even a blind hog finds an acorn, every now and then."
-
-
-
Sometimes questionnaire responses generate results that are certainly real, but for which an answer is not immediately apparent. Sometimes information from another question in our survey, can be used to better understand. To shed light as well as heat. Here's an example:
Smoking
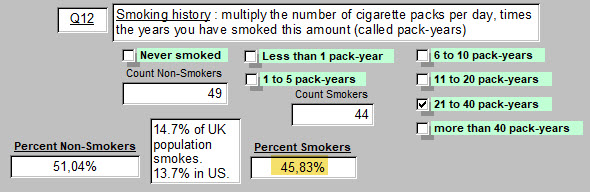
Here are responses to Question 12, about smoking history of respondents. This particular respondent has a smoking history of 21 to 40 pack-years.
51% are Non-Smokers. 46% smoked in the past or still do.
In the UK, 14.7% of the population smokes. USA 13.7% of the population smokes, as seen above.
So there already a question is forming. There are more smokers in this sample of the population that presents with "Long-term" COVID-19, than in the population.
As a past Professor of Neuroanatomy used to say: "Why? ... We do not know."
Next
Do Non-smokers and those with a Smoking History experience a different balance of Physical and Emotional "brokenness"?
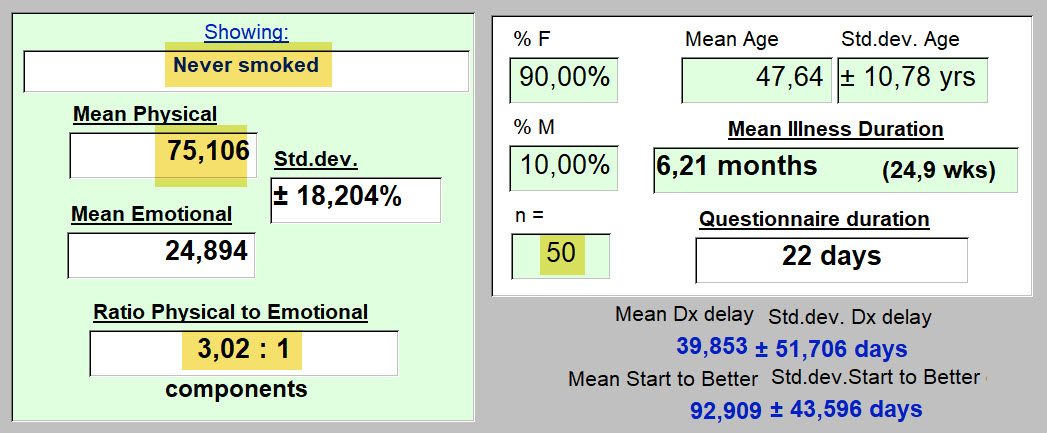
First, the Non-Smokers:
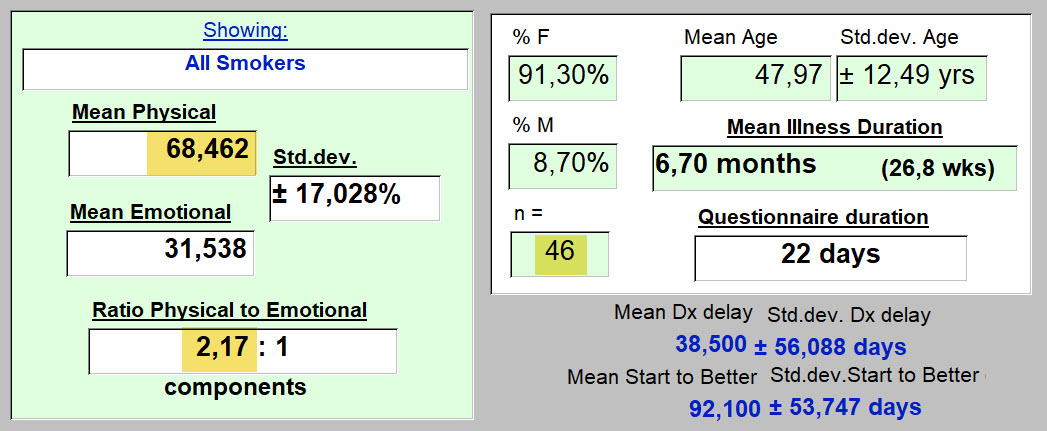
Next, the Smokers
Interpretation :
-
-
- Those who do not smoke, have a different balance of Physical and Emotional symptoms than do smokers. Non-smokers have on average 75% Physical Symptoms and 25% Emotional. Smokers, 68.5% Physical and 31.5% Emotional. Some would say: "Pretty close." As more responses come in, we'll see how this result changes.
- But perhaps we already have enough responses to hint at an answer. To be robust enough to tolerate a statistical onslaught.
- And if their is a difference an appropriate answer may still be: "Why? We do not know ..."
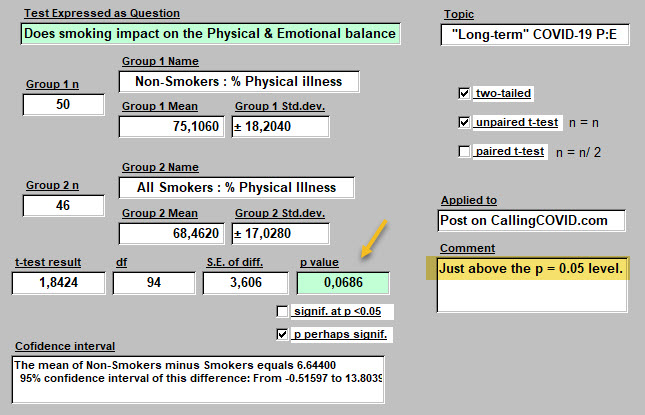
- Is this suggested difference in mean % Physical values real? Here comes the test ...
-
The difference generates a p value of about 0.07. That means there are about 7 chances in 100 that the apparent difference discovered in Smokers compared with Non-Smokers in the mean %Physical to % Emotional Balance is not real and arose by chance. Since 7 out of 100 is not much chance, I'd bet on our hypothesis that Smokers and Non-Smokers live this illness slightly differently.
To see if this holds, a few more responses would help to confirm that this subtle difference is real.
Why would this be? What has smoking done to change this rapport? "Why? ... we do not know."
So what's the point?
-
-
- That all those suffering with this illness are not perfectly alike.
- That personal habits acquired before becoming infected are today playing a role in recovery.
- Notice that no difference was seen in duration of illness, delay of diagnosis, nor in number of days from start of illness to when starting to feel better.
- That methods exist for finding and confirming actual differences in what, at first glance, looks like a uniform population of "Long-term" COVID-19 sufferers. When looked at a little more carefully, one finds different sub-groups. These add to our understanding of this illness. Even in illness, we are each individuals.
-
CONCLUSIONS
For both women and men with this illness,
-
-
- Physical symptoms can be identified as present
- Emotional symptoms can be identified as present
- Besides gender, other personal habits impact on how Physical and Emotional components of this illness are perceived. (Smoking or not).
- While there is a balance between the two that varies from one person to the next, on average for what this specific illness effects or "breaks" is 72% physical and 28% emotional. Is this different than the response to any other serious illness? But trying to convince oneself that it's all one or the other, is wrong we have seen, and probably won't work. Might delay healing.
- The number of defects or deficits distancing respondents from a desired state of unified health, are usually very numerous for these particular patients (i.e., many physical symptoms reported). Perhaps unusual from what happens most offen in Medicine. (Think of appendicitis, a heart attack, a breast cancer, pulmonary embolism, a broken femur, an itchy rash). This is a multi-system disease. (Reminiscent of a car accident victim who has sustained a multi-trauma set of injuries).
- While some will suggest that a treatment for the physical components of this illness is lacking (several still experimental under clinical study have suggested effectiveness, and vaccines a promise for the future), that is not true for the host of psychologic symptoms that are manifesting each day in these responses.
- And yet, use of available therapies in that domain at a professional level are not being frequently sought, preferring to relie on other sources scored higher as potentally effective for emotional support.
- Most individuals having symptoms of a broken leg (not actually studied here), would not hesitate to seek aide from a source beyond family and friends, to get that painful problem fixed. A whole constellation of painful emotional symptoms were uncovered through this questionnaire. And yet, the hesitation for moving promptly towards professional help is all too evident in the responses. Identifying why is a very essential next step.
- Is effective care in the setting of this exact 72:28 balance of physical and emotional symptoms on this day, being obtained from "healthcare"? If not, what's missing? There are just too many broken souls out there to keep wearing blinders like my horse used to do. Come on my fellow physicians: take off those blinders and see your patient. Perhaps for the first time.
-
Presented again below are quotations from the respondents. These are their responses to the question which is phrased as follows in the questionnaire:
"Time now to listen to you directly. To hear your new found expertise with COVID-19.
If you could offer a few words of advice to those from whom you sought care during this illness, what would you say?"
Here is what some wrote ...
(75 responded, 21 skipped this opportunity to write any thoughts, as of Oct. 4, 2020).
Where would the following thoughts have come from?
I have to assume, from what they experienced and were made to feel in their exchanges with "the System."
These have not been subselected for effect. Some convey a positive response to exchanges with "healthcare." Most do not.
--------
"Listen and don’t dismiss."
"This is not just anxiety, its not all in our head, we are suffering, hundreds of thousands of us who never got better. Do your jobs and help us instead of accusing us of being crazy hypochondriacs!"
"Listen, try to understand and show empathy. If you are not an expert, refer to someone who may be! It's ok not to have the answers but don't be dismissive."
"Believe me, be sympathetic, refer me to specialists."
"Keep researching, keep looking for answer and be honest and transparent where you don't know. I wouldn't be seeking your help if I wasn't suffering."
"LISTEN to your patient, and BELIEVE them."
"Try to understand what the illness is like for me."
"I have very few words. I lost all faith in providers after this experience. The total lack of care, compassion, and guidance of the doctors was traumatic in itself."
"See us face to face and perform tests to find out what is going on in our body rather than playing guessing games."
"Medical profession need to be up to speed with long Covid."
"Please take time to read the newest studies, research, and articles written by those struggling. We don’t expect you to have the answers but we do expect you to listen, believe, educate yourself and advocate for us."
"Thank you to those who believed me - particularly my close family and my doctor, and therapists I have sought help from."
"... just listen, were not mad!"
"Listen more. Seek answers, it's what we who suffer need in order to improve. We won't all "get better in time", some have physical ailments as a result of the virus."
"Be patient."
"Don't put everything down to anxiety."
"Listen to the patient. You may have concerns for their breathing but other symptoms are also worrying for us. Those other symptoms may also point in a direction you hadn’t considered especially if tests come in normal."
"Listen to your patient as they know how they feel. Support the patient even if there isn't any treatment."
"Admit you dont know but continue to learn."
"Be open-no preconceived boxes for symptoms and treatments."
"Please believe your patients, and let them know you believe them, - show empathy even if you don’t understand how one virus can cause such a toll or wide range of symptoms."
"Remember it could be you."
"Listen, empathy, believe us."
"You didn’t know enough. I don’t blame you for that. But you didn’t try hard enough to learn from emerging sources. I blame you for that. You were overworked. I don’t blame you for that. You didn’t make sure I was checked on and you left my loved ones to support me on their own. I blame you for that. You made light of my suffering. That hurt. I will never trust the NHS again. I will do everything I can to never have to talk to healthcare professionals for the rest of my life."
"...slow down and LISTEN and look."
"Listen to us. Do more."
"Believe, listen, offer tests to exclude other issues, reassure even if all tests show nothing, that this is real. Advise to rest and convalesce."
"Listen, believe, Learn, care, respect and keep in touch even if you cannot do much."
" keep up the good work "
"Keep listening to the patients. We will be the ones giving you answers for a better research and care."
"Empathy goes a long way, especially if it is phone consultation. It would have been helpful if doctors had checked in on me, rather than me doing it once a month when my sick note ran out. It was hard to speak to 12+ doctors over the past 5 months, a consistent doctor/small group of doctors if more practicable would have been better."
"Listen to your patients, give them at least the allotted time, read the research and leave no stone unturned. Remember your clinical judgement rather than putting so much weight on lab tests and assess new symptoms as you would without Covid."
"Be open minded and keep looking for answers."
"You needed to listen and be much more supportive and understanding."
"Listen to symptoms, focus on clinical experience and use the two to find creative care solutions."
"I am very very lucky to have access to excellent medical care, doctors who are researching this virus to better help their patients and I know how rare this is!"
"Should have looked up my medical history/listened /believed me in the beginning."
"... algorithms are useless. You are medically trained for what? To look at a screen and find out about a disease that is too new for systems and bureaucracy. The answers lie with your patients and educating yourselves. Ignore the 'machine and do what you first got into the profession for. Helping people."
"It would have been helpful if you had not just listened, but actually heard when I was saying. To not be so insensitive and judgemental; blaming all my symptoms on being overweight and my mental health. To please try and treat me holistically and not just separating out symptoms. To actually do some reading and a bit of research about long covid and to see that I am not making this up. I wish you had made me feel validated instead of being left sad and frustrated."
"Don't treat us as imagining we are ill, help us."
"I know not any one has answers yet but TRY SOMETHING."
"I mostly have had positive experiences."
"Don't be dismissive of concerns of those who consult you. This includes taking complaints of particular ailments seriously even if they are not present at the time of the consultation."
"Don’t be afraid to say “we don’t know” - that is a sign of intelligence to me. Express you believe what I’m telling you directly to me. I can tell you do, but that affirmation is soothing. Instruct ALL staff to wear masks correctly ALL the time. Most do, but I did encounter a few who wore it below their nose. Please REQUIRE AND ENFORCE requirement on wearing masks. If someone won’t don’t see them. Online support groups are not for everyone, but offer that information to your patients. My PCP puts an update about local Covid stats, what they mean, trends, and updates on clinical studies."
"Be able to say you don't know share resources / talk to other doctors and give your patients that benefit of the doubt no one knows what this thing is quite yet.. Keep your politics out of my health care!"
----------------
As you read through the above, certain responses for advice to healthcare providers may have caught your attention more than others. You may even have found a favorite.
Mine is: "Remember it could be you."
And that, because it's quite true.
----------
This has been Lesson 7: It's Physical, It's Emotional. It's Both.
Here is a link back to the previous lessons emerging from these preliminary results.
An Introduction to the Questionnaire.
<<<<<<<< Home
A découvrir aussi
- Lesson 1: Test results - how uncertainty changes our lives
- Lesson 5: Fostering resilience
- BIO: Principle Investigator