Lesson 3: Effective emotional support - where shall we turn?
CallingCOVID.com
Thanks for visiting!
To translate this page, select your
language from the dropdown menu below:
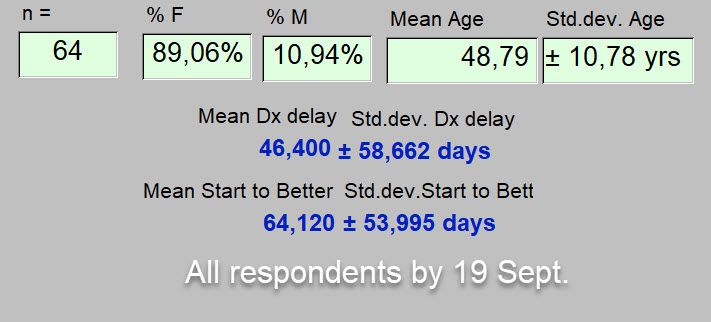
Our current questionnaire attempts to capture various aspects of the emotional components of this COVID-19 illness. It is ongoing, and on September 19 had received 64 completions.
Of course most, if not all illnesses, have emotional components.
If you have "long-term" COVID-19, consider taking our questionnaire before reading on.
That will make your answers much more meaningful for you and us. The questionnaire, and a link to it, are introduced here.
----------
In this article we will present some of the preliminary results from this questionnaire.
Who responded?
As one can see above, most of the respondents were female. Since this was a strong majority, one must wonder if "long-term" COVID-19 behaves in this way beyond the confines of our questionnaire.
One can see the average age. At present, no responders have been younger than 21 years old,
nor older than 74 years.
Though not shown here, these responders to the questionnaire have been living with this illness for an average of 6.42 months (25.7 weeks). These values being the difference between the date the questionnaire was responded to, and the date when this illness was felt to have begun. That's a long time to be sick.
From a healthcare perspective it should be underlined that from when the patient was first symptomatic to when diagnosed with this illness, was an average of 46 days. As illnesses go, that delay of diagnosis is quite long. It will be addressed elsewhere. The other result of note is that from start of illness to when the patient began to feel better is an average interval of 64 days.
42% of the respondents were 48 years old or younger, with a mean age of 39 years. Once again, the results show a female predominance for this illness in this age group as well.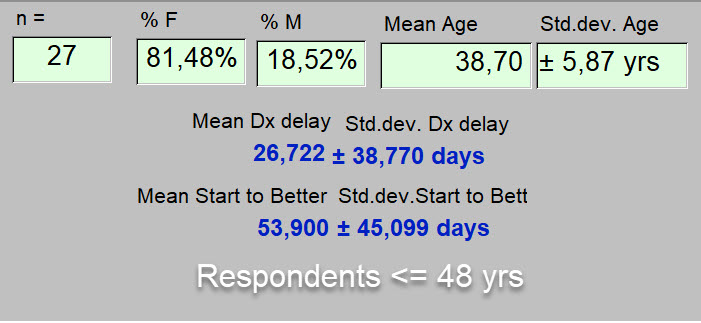
Let's compare that with the older respondents, 58% of those who completed the questionnaire.
These preliminary results suggest an even stronger female predominance to this illness in this age group, having an average age of 56 years.
In comparing the younger and older populations here, one also discovers a longer delay in diagnosis (p=0.0239), and a longer period of living with this illness from when it began to when the respondent first felt better (p = 0.2098) in the older group. This latter difference was not statistically significant, but may still be quite real. And as additional responses come in, such differences between younger and older patients may be easier to distinguish. Be that as it may, all these intervals of illness are indeed "long-term" for what is too often presented as an acute illness.
Now that we know a bit more about this sample of respondents to the questionnaire, let us focus on the topic for this article.
This illness like most, has an emotional component.
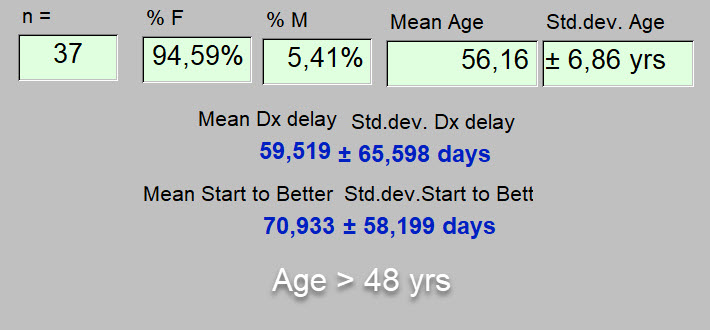
Can one define a balance between those aspects of this illness that are physical and those that are emotional? We address that with the question below.
Response?
As one can see at the bottom of the above graphic, only 14% felt that this illness was 100% physical. 31 respondents placed it as 80% physical and 20% emotional, and 17 felt that the emotional and physical components were equal. No one thought is was completely emotional.
------------
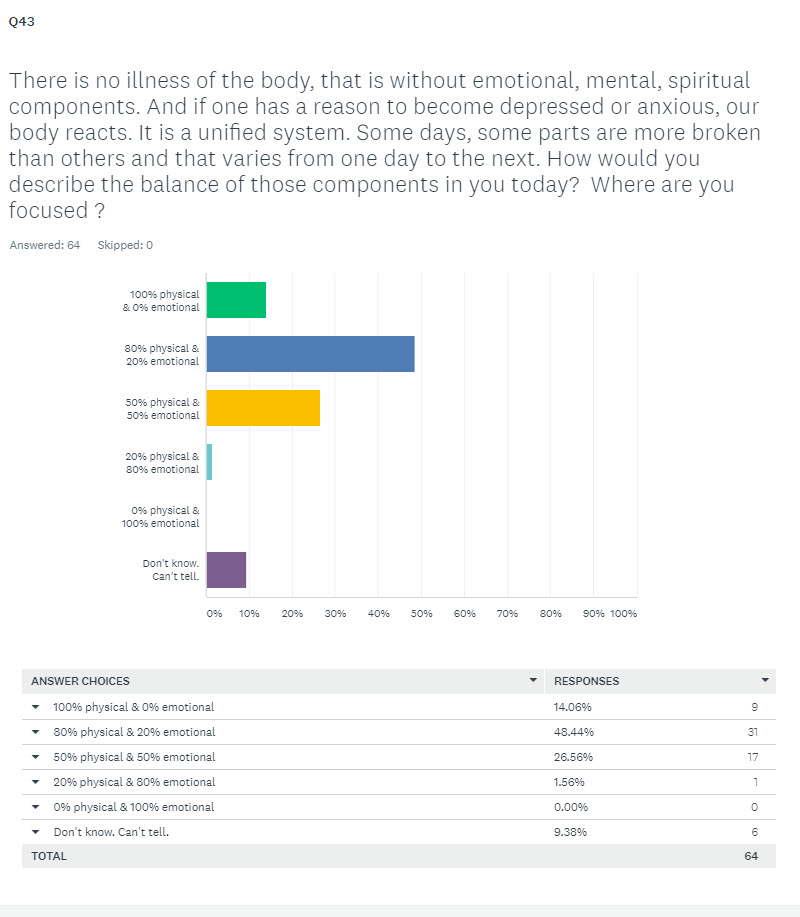
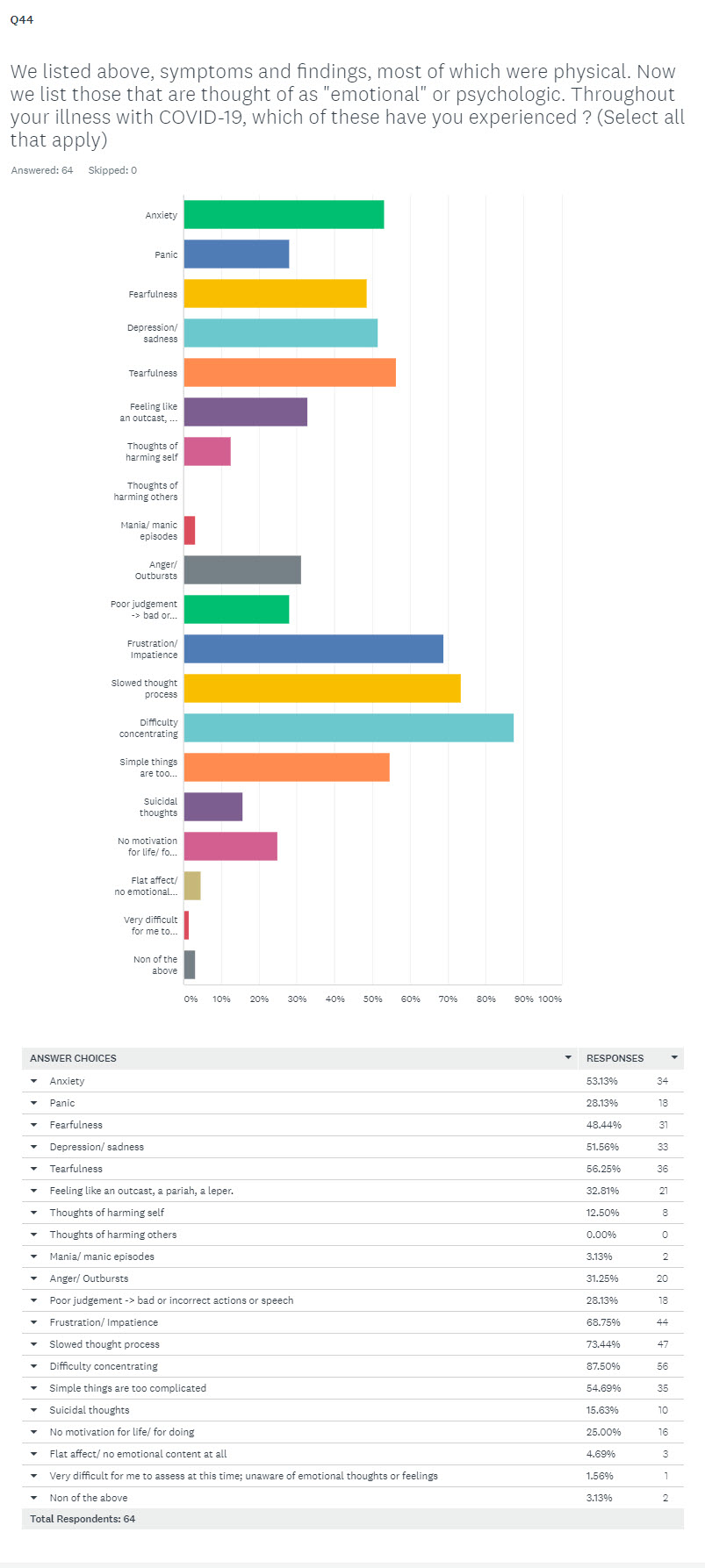
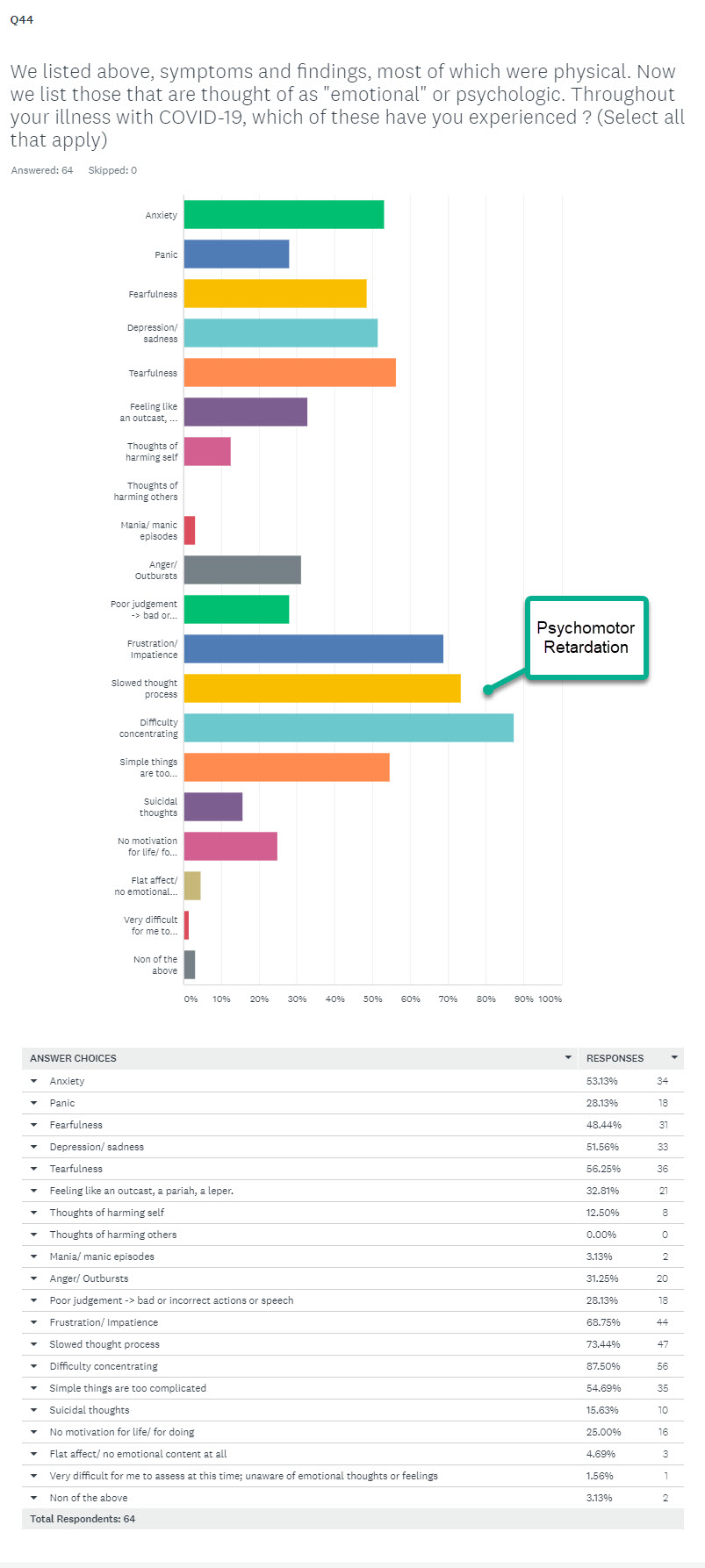
Which emotional symptoms were experienced?
Respondents could select as many as they wished from the provided list.
Though not presented here, by respondent, most respondents selected several symptoms. These are presented below, followed by a table of frequencies of responses obtained.
Below, we have stuck a label on some emotional symptoms experienced more frequently in this sample.
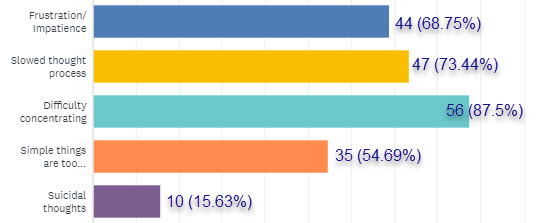
To focus in just a bit more, there was a group of emotional symptoms in the middle of this list that had a greater frequency of responses as mentioned. These can be listed under a heading of "psychomotor retardation," a finding often associated with depression but also other psychological illnesses.
One can readily see from the above percentages that these were not rare events.
A response that was less common was for suicidal ideation. Though less common, this is always concerning. If the respondents who provided this response are still feeling this way, they must take it seriously, and contact someone as soon as possible to help manage that.
"Psychomotor retardation"
The term implies the finding of a significant delay in both thought and action, or converting thought into an action. For example: "Oh no! That lightbulb just blew! I guess I'll have to change that. I guess I'll have to find where the light bulbs are stored, bring one out, and find a way to get up there and change the bulb. Frankly, I don't think I can do that. Frankly, right now, that's just too much for me. Let's just wait. Let's quietly think about this just a bit more."
It might also be as simple as a delay in converting a thought in one's head, into speech if that is what is required. For example: a significant delay when answering questions.
------------
So if these problems do in fact exist for those with "long-term" Covid -19, where are these patients finding a source of emotional support?
We looked at five such potential sources:
- family of the respondent
- healthcare providers
- a professional therapist, or someone felt to provide a therapeutic role for the respondent
- online contacts and groups
- personal habits, hobbies, and practices
We thought about including pets as a source of emotional support. Many respondents when answering the question about listing daily activities, included time with pets.
We decided against its inclusion to simplify data retrieval, analysis and especially, to make presentation of results a bit more concise.
We also decided against its inclusion prompted by an underlying concern that the pet dogs, cats and turtles, might accrue more points for effectiveness, than the healthcare providers.
----------
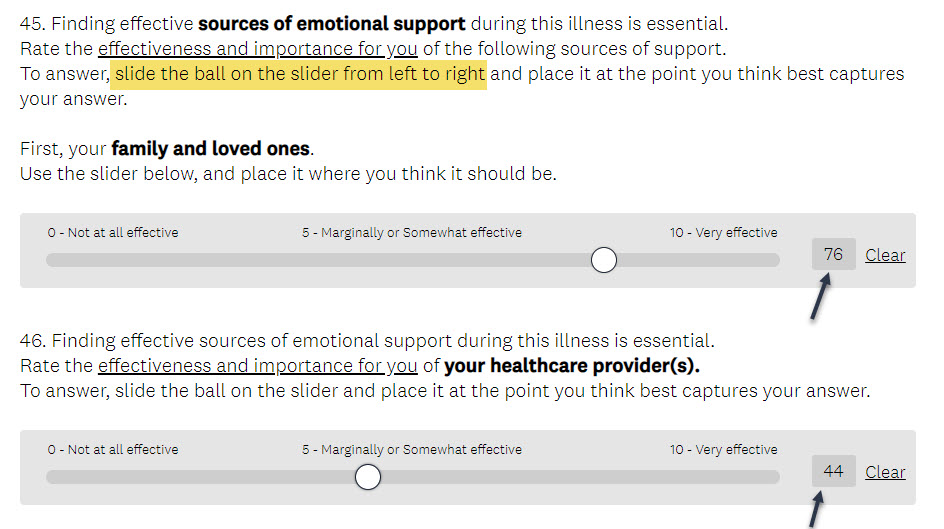
Here's an explanation of how a quantitative response was obtained for each of these sources.
As shown below, in answering the respondent moved a slider from left to right on a scale presented as:
0 - Not at all effective
5 - Marginally or somewhat effective
10 - Very effective.
This motion of the slider was converted into a value of 0 to 100.
We'll call this the "Effectiveness Score."
So above one can see a score of 76 for the families effectiveness in providing emotional support, and below that, a score of 44 for the healthcare provider in providing emotional support for this person ill with "long-term" Covid-19.
If one of these sources of emotional support did not exist for the respondent, she or he could simply skip the response and move to the next question.
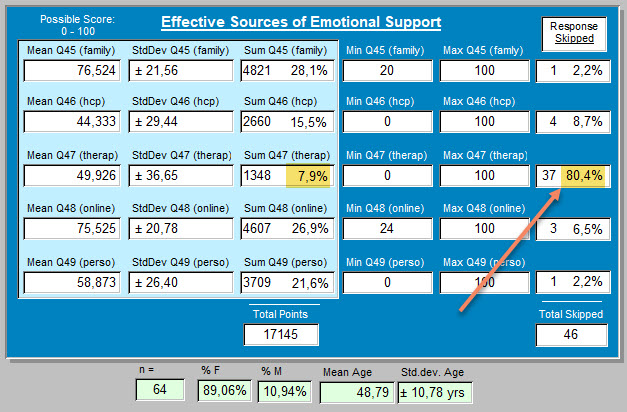
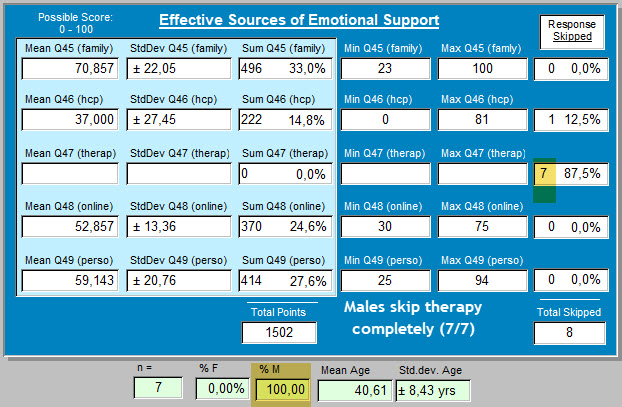
For the 64 respondents up till September 19, they showed a very informative result.
80% skipped over "therapist" as a source of emotional support.
Let's get into that just a bit more.
We have seen that females are more frequently involved than males with this "long-term" Covid-19.
Yet 30 of 57 women skipped the question about therapists as emotional support.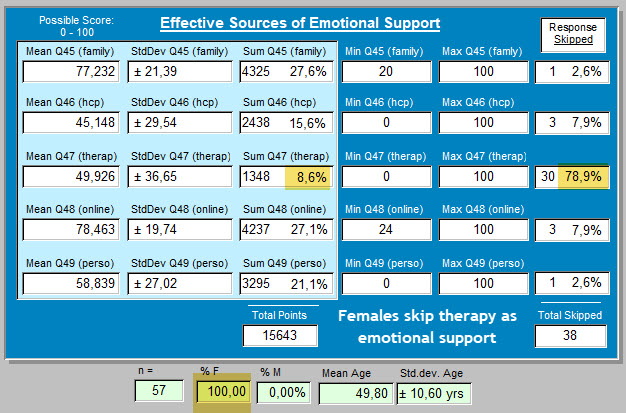
It was much easier to quantify this for male respondents.
None, 0%, scored the therapist as source of emotional support. 100% skipped over this as seen below.
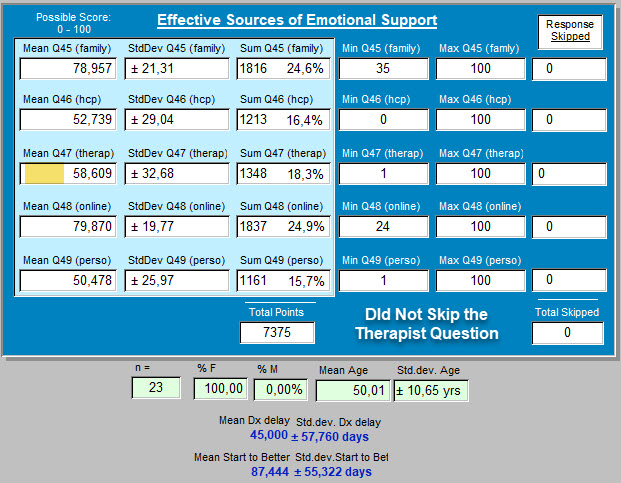
For those respondents who did not skip the choice of therapist as potential sources of emotional support, the results are given below. On that slider explained above (0 -> 100), the "therapist" choice
determined an average score of 58.6.
Let's look a bit closer at the scores obtained by respondent age.
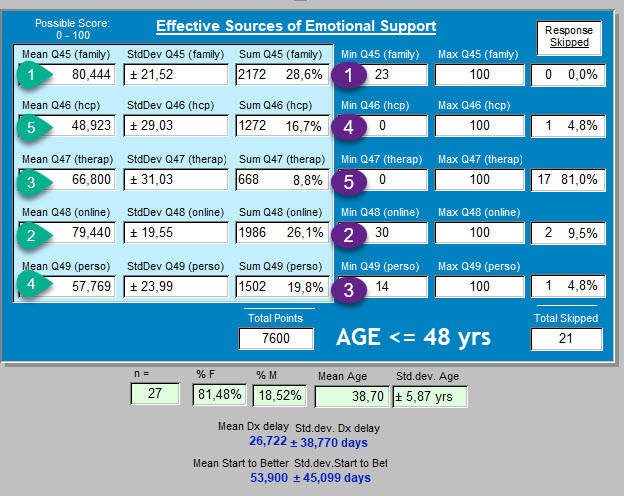
First, for respondents 48 years old and younger.
In the first column on the left are the average scores for each of the five categories of emotional support.
Again, this was done with the slider when responding, giving a score range of from 0 to 100.
So the winner, if you will, for the source of support most important on average for these 27 respondents age 48 yrs and less, was: "family."
Second on the podium of effective emotional support: "online contacts and groups." These beat out,
the "therapist" with an average of 67 points awarded.
"Personal habits, hobbies and practices" were next in order as perceived sources of emotional support.
And in last place (at least for these five) were "healthcare providers."
If one looks at the results in the third column from the left (with the purple numbers) one is looking at the sum of the scores awarded, as opposed to mean values. This permits compensating for when choices were not made but skipped over.
Once again, "family" comes in at first place, as most effective source of needed emotional support.
Placing those data here may make it easier than with the above graphic:
Rating of effective sources of emotional support:
-
- Family (28.6% of points awarded)
- Online contacts and groups (26.1% of points)
- Personal habits, hobbies, & practices (19.8%)
- Healthcare providers (16.7%)
- Therapists (8.8%)
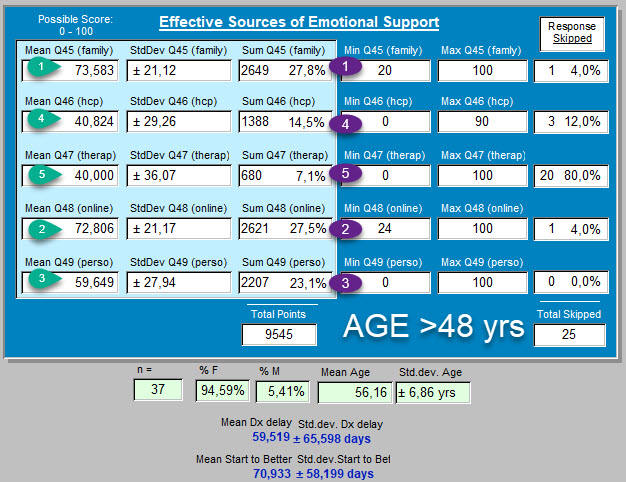
Below are the results for respondents older than 48 years.
The numbers change slightly but not the outcome. The same rating as given above emerges.
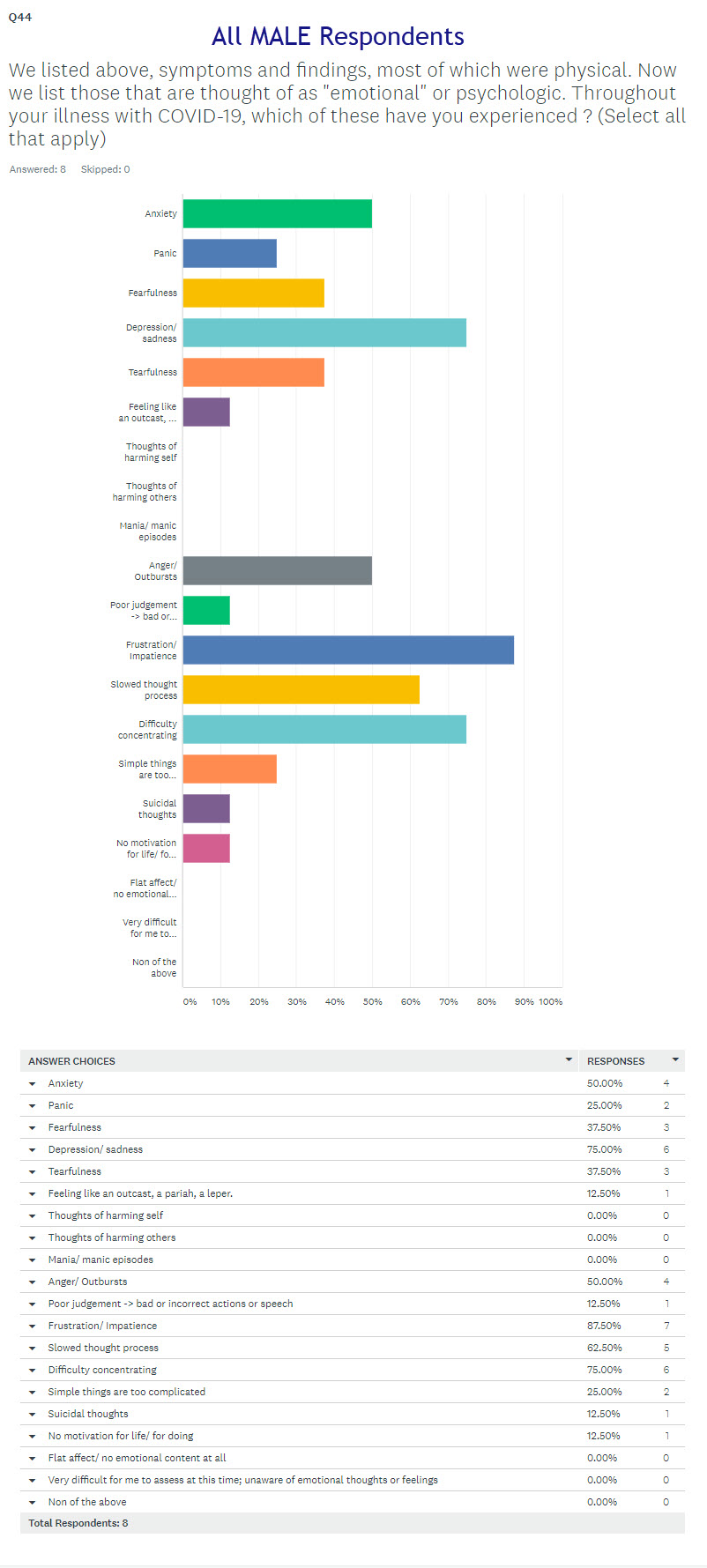
Such results engender many thoughts.
Here are a few:
Perhaps male respondents skipped over the choice of "therapists" for emotional support, because they did not feel the presence of any important emotional need or problem.
As we can see below, that was not the case.
It is important to remind that this subset of our 64 respondents is pretty small. Nevertheless, it does confirm that psychological issues have been present for men as part of their illness with COVID-19, or at least during that time that this illness has been present. And not shown here, their responses for before the illness began suggested no such problem felt to be present.
The data do not permit any comment about potential differences between men and women about how and when and from whom, they seek emotional support. But the needs for support seem shared and universal.
Next point: Finding emotion amid the electrons.
"Online contacts and groups" garnered position number two as an effective source of emotional support. After family support, this was felt to be a more effective source of emotional support than the respondent's personal habits, healthcare providers, or therapists.
This may be a bit shocking, and especially for those in healthcare.
This result also points to the limitations of these preliminary data. As mentioned before, 64 respondents is still a relatively small number when trying to draw conclusions from a questionnaire. (Remind those you know with "long-term" COVID-19 to complete the questionnaire please !)
More importantly, this result points to a certain selection bias for this questionnaire.
- It is offered to respondents, online.
- It is respondent to, online.
- And now we are sharing preliminary work results, again online.
- Dividing this group of respondents by age did not displace this response in favor of online groups from its number two position. So it's not an age phenomenon, in which "the young" depend on and seek out others online for support, but "the old" (nhaving not been raised to be computer geeks), do not. These are all, computer geeks.
Of course 20 years ago, that response choice would not have appeared in such a questionnaire about various aspects of an illness.
But up until today, we have not printed up and distributed the questionnaire from house to house, or by mail to those with "long term" - COVID-19. We probably won't. But we can't say that the answers, might not be different. Especially for that "online contacts and groups" response. So that is a limitation or sample bias of our questionnaire.
Next point : Find a way to make therapy happen at a professional level
Let's put some of these observations together.
Psychological or "emotional" findings are present here in the answers of the respondents.
They are present in females, some of whom but not many, turn to "therapists" for emotional support.
They are present in males, none of whom responding so far to the questionnaire, did other than to skip over this choice.
Yet that need seems present. And professionals in psychology and psychiatry are available.
Without being addressed in this questionnaire, if accessibility to the sources of emotional support are currently less available due to actual methods of financing these interventions found in the present healthcare system, then that system is badly broken and should be repaired as soon as possible.
Other reasons that contribute to separating therapist and those who need therapy should also be sought. We may have some other ideas. That's not our job here today.
It cannot be emphasized enough when one encounters in some respondents, the presence of suicidal ideation, that needs immediate attention. That response represents a call for help that must not be ignored.
Next point: In this questionnaire, "Healthcare" took a beating.
Is it time to bring back 'old-fashioned Medicine', or not yet?
If responding to this questionnaire was the first time that the question about suicidal ideation was posed, in individuals most of whom had contact with the healthcare system and its providers, and no one in that system asked the question, another glaring inadequacy has been uncovered.
Of course that inadequacy has been more than hinted at by these preliminary results.
Effectiveness of "healthcare provider" for emotional support ?
"Healthcare provider" as the person to turn to when one needs emotional support during this illness is here in fourth position out of five. Before turning to their physician these respondents prefer to talk to each other online and compare anecdotes, to pursuing a diagnosis in that healthcare setting.
After first talking it over with the family members, they may try to rely on their personal habits, hobbies, or practices to bring them up out of emotional doldrums. Some may even try to develop new habits, perhaps yoga or diet change or reiki.
The coronavirus may be "novel" or new. But healthcare, or Medicine as it used to be called, is not new. And it's job has always been to name the disease that is responsible for the patient's misery. To give it the correct name, which is called a diagnosis, and to offer therapy when available. For quite some time, as it tried to accomplish these tasks, Medicine did have more success, when compared with exchanging anecdotes over the fence in the backyard, or even now online. It was usually more efficient than developing new personal habits (these take time, and many illnesses don't). In the past, Medicine even supplied emotional support for the patient. It was a form of compassionate care. It frequently supplied 60% of a good outcome from illness, even on the Surgical Wards.
Perhaps the numerical results presented here exaggerate the problem. After all, 14% of the respondents so far did suggest that this was 100% a physical problem, without any emotional component. That's a mathematical minority of the respondents.
But let's move away from the numbers and see what respondents are actually saying about their contact with the healthcare system and its providers, while their present illness was being evaluated and treated.
Again, these are quotations from the respondents. These are their responses to the question which is phrased as follows in the questionnaire:
"Time now to listen to you directly. To hear your new found expertise with COVID-19.
If you could offer a few words of advice to those from whom you sought care during this illness, what would you say?"
Here is what some wrote ...
(and some did skip this opportunity to write any thoughts).
Where would the following thoughts have come from?
I have to assume, from what they were made to feel in their exchanges with "the System."
--------
"Listen and don’t dismiss."
"This is not just anxiety, its not all in our head, we are suffering, hundreds of thousands of us who never got better. Do your jobs and help us instead of accusing us of being crazy hypochondriacs!"
"Listen, try to understand and show empathy. If you are not an expert, refer to someone who may be! It's ok not to have the answers but don't be dismissive."
"Believe me, be sympathetic, refer me to specialists."
"Keep researching, keep looking for answer and be honest and transparent where you don't know. I wouldn't be seeking your help if I wasn't suffering."
"LISTEN to your patient, and BELIEVE them."
"Try to understand what the illness is like for me."
"I have very few words. I lost all faith in providers after this experience. The total lack of care, compassion, and guidance of the doctors was traumatic in itself."
"See us face to face and perform tests to find out what is going on in our body rather than playing guessing games."
"Medical profession need to be up to speed with long Covid."
"Please take time to read the newest studies, research, and articles written by those struggling. We don’t expect you to have the answers but we do expect you to listen, believe, educate yourself and advocate for us."
"Thank you to those who believed me - particularly my close family and my doctor, and therapists I have sought help from."
"... just listen, were not mad!"
"Listen more. Seek answers, it's what we who suffer need in order to improve. We won't all "get better in time", some have physical ailments as a result of the virus."
"Be patient."
"Don't put everything down to anxiety."
"Listen to the patient. You may have concerns for their breathing but other symptoms are also worrying for us. Those other symptoms may also point in a direction you hadn’t considered especially if tests come in normal."
"Listen to your patient as they know how they feel. Support the patient even if there isn't any treatment."
"Admit you dont know but continue to learn."
"Be open-no preconceived boxes for symptoms and treatments."
"Please believe your patients, and let them know you believe them, - show empathy even if you don’t understand how one virus can cause such a toll or wide range of symptoms."
"Remember it could be you."
"Listen, empathy, believe us."
"You didn’t know enough. I don’t blame you for that. But you didn’t try hard enough to learn from emerging sources. I blame you for that. You were overworked. I don’t blame you for that. You didn’t make sure I was checked on and you left my loved ones to support me on their own. I blame you for that. You made light of my suffering. That hurt. I will never trust the NHS again. I will do everything I can to never have to talk to healthcare professionals for the rest of my life."
"...slow down and LISTEN and look."
"Listen to us. Do more."
"Believe, listen, offer tests to exclude other issues, reassure even if all tests show nothing, that this is real. Advise to rest and convalesce."
"Listen, believe, Learn, care, respect and keep in touch even if you cannot do much."
" keep up the good work "
"Keep listening to the patients. We will be the ones giving you answers for a better research and care."
"Empathy goes a long way, especially if it is phone consultation. It would have been helpful if doctors had checked in on me, rather than me doing it once a month when my sick note ran out. It was hard to speak to 12+ doctors over the past 5 months, a consistent doctor/small group of doctors if more practicable would have been better."
"Listen to your patients, give them at least the allotted time, read the research and leave no stone unturned. Remember your clinical judgement rather than putting so much weight on lab tests and assess new symptoms as you would without Covid."
"Be open minded and keep looking for answers."
"You needed to listen and be much more supportive and understanding."
"Listen to symptoms, focus on clinical experience and use the two to find creative care solutions."
"I am very very lucky to have access to excellent medical care, doctors who are researching this virus to better help their patients and I know how rare this is!"
"Should have looked up my medical history/listened /believed me in the beginning."
"... algorithms are useless. You are medically trained for what? To look at a screen and find out about a disease that is too new for systems and bureaucracy. The answers lie with your patients and educating yourselves. Ignore the 'machine and do what you first got into the profession for. Helping people."
"It would have been helpful if you had not just listened, but actually heard when I was saying. To not be so insensitive and judgemental; blaming all my symptoms on being overweight and my mental health. To please try and treat me holistically and not just separating out symptoms. To actually do some reading and a bit of research about long covid and to see that I am not making this up. I wish you had made me feel validated instead of being left sad and frustrated."
"Don't treat us as imagining we are ill, help us."
"I know not any one has answers yet but TRY SOMETHING."
"I mostly have had positive experiences."
"Don't be dismissive of concerns of those who consult you. This includes taking complaints of particular ailments seriously even if they are not present at the time of the consultation."
"Don’t be afraid to say “we don’t know” - that is a sign of intelligence to me. Express you believe what I’m telling you directly to me. I can tell you do, but that affirmation is soothing. Instruct ALL staff to wear masks correctly ALL the time. Most do, but I did encounter a few who wore it below their nose. Please REQUIRE AND ENFORCE requirement on wearing masks. If someone won’t don’t see them. Online support groups are not for everyone, but offer that information to your patients. My PCP puts an update about local Covid stats, what they mean, trends, and updates on clinical studies."
"Be able to say you don't know share resources / talk to other doctors and give your patients that benefit of the doubt no one knows what this thing is quite yet.. Keep your politics out of my health care!"
----------------
This seems like the perfect spot to bring this to an end.
In the past, a term called "hysteria" was used to describe symptoms a patient presented with that have no physical or other findings to support the complaints. The root origin of the word is for the Latin term for "uterus," so, you guessed it ... most were women.
People (especially patients) didn't like the term. SIgmund Freud when studying neurology quickly learned about that resistence. He renamed it "conversion reaction," and defined that term quite thoroughly in his writings. Essentially, he thought that these patients had repressed emotional thoughts, and then "converted" those unconscious thoughts, without even knowing that they were doing it, into physical aches and pains.
But more often, and in his best cases studied and described, the symptoms were neurologic, and often paralyses: couldn't walk. Couldn't move, Couldn't raise an arm, or look to the left, or turn head to right.
In children, this "hysteria" often presents as gait distrubances; dragging a leg, or saying that it hurts to walk or do stairs. And yes, some of those with these complaints do present the diagnosis Freud invented. They have repressed emotional problems. It's real. They can be treated. Good results are usually obtained.
Is that what's going on here?
Very, very unlikely. The symptom lists don't match up with what Freud, and others since, have defined and presented.
But Freud's work in this does teach something very applicable here.
He emphasized the importance of really, really taking the time to listen carefully to the patient.
He gave examples of how rushing it just doesn't work.
"Gehen Sie schnell vor und Sie werden etwas vermissen. Sie werden den wichtigsten Teil verpassen."
"Proceed quickly, and you'll miss something. You'll miss the most important part."
In approaching those with "long-term" COVID-19, that is an essential lesson, and should be incorporated in practice behavior.
-----------
If a person reading this is suffering from "long-term" Covid-19, if nothing else please draw from this that you are not alone.
In a previous article on symptoms and tests found in this illness, those lists are quite long. They capture the widespread suffering that this illness imposes on a human body. Here today, in this preliminary review of results, we have also tried to bring attention to the fact that this illness imposes widespread suffering on the emotions as well.
After receiving more responses Lesson 7: It's Physical. It's Emotionl. It's Both was written on October 4, and explores the balance "Long-term" COVID-19 patients find between Physical and Emotional symptoms. And yes, both are present.
Those in need of effective emotional support for this illness, and those who can provide it, should be on the same team. Not on opposing teams.
If these preliminary results, and hopefully the many that will follow (hint! ), can succeed in conveying that message to those on both sides of the exam table, that would be a quite positive result. Let's remain hopeful.
The goal of those treating illness used to be "to relieve suffering, and heal the sick where possible."
In fact, today the goal probably remains the same. But if too many things now separate patient and healer, those things should be sought after, identified, and moved aside. They get in the way. They take up time.
Otherwise, with or without "long-term" COVID-19, we may all be in a world of trouble.
- Questionnaire Answers page
- Questionnaire Answers : Start Here
- Lesson 1: Test results - how uncertainty changes our lives
- Lesson 2: So what about that weight gain?
<<<<<<<< Home
A découvrir aussi
- Questionnaire Answers : Start Here
- Lesson 1: Test results - how uncertainty changes our lives
- BIO: Principle Investigator